Rheumatoid arthritis
| Rheumatoid arthritis | |
|---|---|
 | |
| A hand severely affected by rheumatoid arthritis. This degree of swelling and deformation does not typically occur with current treatment. | |
| Specialty | Rheumatology, Immunology |
| Symptoms | Warm, swollen, painful joints[1] |
| Complications | Low red blood cells, inflammation around the lungs, inflammation around the heart[1] |
| Usual onset | Middle age[1] |
| Duration | Lifelong[1] |
| Causes | Unknown[1] |
| Diagnostic method | Based on symptoms, medical imaging, blood tests[1][2] |
| Differential diagnosis | Systemic lupus erythematosus, psoriatic arthritis, fibromyalgia[2] |
| Medication | Pain medications, steroids, Nonsteroidal anti-inflammatory drugs, disease-modifying antirheumatic drugs[1] |
| Frequency | 0.5–1% (adults in developed world)[3] |
| Deaths | 30,000 (2015)[4] |
Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects joints.[1] It typically results in warm, swollen, and painful joints.[1] Pain and stiffness often worsen following rest.[1] Most commonly, the wrist and hands are involved, with the same joints typically involved on both sides of the body.[1] The disease may also affect other parts of the body, including skin, eyes, lungs, heart, nerves, and blood.[1] This may result in a low red blood cell count, inflammation around the lungs, and inflammation around the heart.[1] Fever and low energy may also be present.[1] Often, symptoms come on gradually over weeks to months.[2]
While the cause of rheumatoid arthritis is not clear, it is believed to involve a combination of genetic and environmental factors.[1] The underlying mechanism involves the body's immune system attacking the joints.[1] This results in inflammation and thickening of the joint capsule.[1] It also affects the underlying bone and cartilage.[1] The diagnosis is made mostly on the basis of a person's signs and symptoms.[2] X-rays and laboratory testing may support a diagnosis or exclude other diseases with similar symptoms.[1] Other diseases that may present similarly include systemic lupus erythematosus, psoriatic arthritis, and fibromyalgia among others.[2]
The goals of treatment are to reduce pain, decrease inflammation, and improve a person's overall functioning.[5] This may be helped by balancing rest and exercise, the use of splints and braces, or the use of assistive devices.[1][6][7] Pain medications, steroids, and NSAIDs are frequently used to help with symptoms.[1] Disease-modifying antirheumatic drugs (DMARDs), such as hydroxychloroquine and methotrexate, may be used to try to slow the progression of disease.[1] Biological DMARDs may be used when the disease does not respond to other treatments.[8] However, they may have a greater rate of adverse effects.[9] Surgery to repair, replace, or fuse joints may help in certain situations.[1]
RA affects about 24.5 million people as of 2015.[10] This is 0.5–1% of adults in the developed world with between 5 and 50 per 100,000 people newly developing the condition each year.[3] Onset is most frequent during middle age and women are affected 2.5 times as frequently as men.[1] It resulted in 38,000 deaths in 2013, up from 28,000 deaths in 1990.[11] The first recognized description of RA was made in 1800 by Dr. Augustin Jacob Landré-Beauvais (1772–1840) of Paris.[12] The term rheumatoid arthritis is based on the Greek for watery and inflamed joints.[13]
Signs and symptoms
[edit]RA primarily affects joints, but it also affects other organs in more than 15–25% of cases.[14] Associated problems include cardiovascular disease, osteoporosis, interstitial lung disease, infection, cancer, feeling tired, depression, mental difficulties, and trouble working.[15]
Joints
[edit]

Arthritis of joints involves inflammation of the synovial membrane. Joints become swollen, tender and warm, and stiffness limits their movement. With time, multiple joints are affected (polyarthritis). Most commonly involved are the small joints of the hands, feet and cervical spine, but larger joints like the shoulder and knee can also be involved.[16]: 1098 Synovitis can lead to tethering of tissue with loss of movement and erosion of the joint surface causing deformity and loss of function.[2] The fibroblast-like synoviocytes (FLS), highly specialized mesenchymal cells found in the synovial membrane, have an active and prominent role in these pathogenic processes of the rheumatic joints.[17]
RA typically manifests with signs of inflammation, with the affected joints being swollen, warm, painful and stiff, particularly early in the morning on waking or following prolonged inactivity. Increased stiffness early in the morning is often a prominent feature of the disease and typically lasts for more than an hour. Gentle movements may relieve symptoms in early stages of the disease. These signs help distinguish rheumatoid from non-inflammatory problems of the joints, such as osteoarthritis. In arthritis of non-inflammatory causes, signs of inflammation and early morning stiffness are less prominent.[18] The pain associated with RA is induced at the site of inflammation and classified as nociceptive as opposed to neuropathic.[19] The joints are often affected in a fairly symmetrical fashion, although this is not specific, and the initial presentation may be asymmetrical.[16]: 1098
As the pathology progresses the inflammatory activity leads to tendon tethering and erosion and destruction of the joint surface, which impairs range of movement and leads to deformity. The fingers may develop almost any deformity depending on which joints are most involved. Specific deformities, which also occur in osteoarthritis, include ulnar deviation, boutonniere deformity (also "buttonhole deformity", flexion of proximal interphalangeal joint and extension of distal interphalangeal joint of the hand), swan neck deformity (hyperextension at proximal interphalangeal joint and flexion at distal interphalangeal joint) and "Z-thumb." "Z-thumb" or "Z-deformity" consists of hyperextension of the interphalangeal joint, fixed flexion and subluxation of the metacarpophalangeal joint and gives a "Z" appearance to the thumb.[16]: 1098 The hammer toe deformity may be seen. In the worst case, joints are known as arthritis mutilans due to the mutilating nature of the deformities.[20]
Skin
[edit]The rheumatoid nodule, which is sometimes in the skin, is the most common non-joint feature and occurs in 30% of people who have RA.[21] It is a type of inflammatory reaction known to pathologists as a "necrotizing granuloma". The initial pathologic process in nodule formation is unknown but may be essentially the same as the synovitis, since similar structural features occur in both. The nodule has a central area of fibrinoid necrosis that may be fissured and which corresponds to the fibrin-rich necrotic material found in and around an affected synovial space. Surrounding the necrosis is a layer of palisading macrophages and fibroblasts, corresponding to the intimal layer in synovium and a cuff of connective tissue containing clusters of lymphocytes and plasma cells, corresponding to the subintimal zone in synovitis. The typical rheumatoid nodule may be a few millimetres to a few centimetres in diameter and is usually found over bony prominences, such as the elbow, the heel, the knuckles, or other areas that sustain repeated mechanical stress. Nodules are associated with a positive RF (rheumatoid factor) titer, ACPA, and severe erosive arthritis. Rarely, these can occur in internal organs or at diverse sites on the body.[22]
Several forms of vasculitis occur in RA, but are mostly seen with long-standing and untreated disease. The most common presentation is due to involvement of small- and medium-sized vessels. Rheumatoid vasculitis can thus commonly present with skin ulceration and vasculitic nerve infarction known as mononeuritis multiplex.[23]
Other, rather rare, skin associated symptoms include pyoderma gangrenosum, Sweet's syndrome, drug reactions, erythema nodosum, lobe panniculitis, atrophy of finger skin, palmar erythema, and skin fragility (often worsened by corticosteroid use).[24]
Diffuse alopecia areata (Diffuse AA) occurs more commonly in people with rheumatoid arthritis.[25] RA is also seen more often in those with relatives who have AA.[25]
Lungs
[edit]Lung fibrosis is a recognized complication of rheumatoid arthritis. It is also a rare but well-recognized consequence of therapy (for example with methotrexate and leflunomide). Caplan's syndrome describes lung nodules in individuals with RA and additional exposure to coal dust. Exudative pleural effusions are also associated with RA.[26][27]
Heart and blood vessels
[edit]People with RA are more prone to atherosclerosis, and risk of myocardial infarction (heart attack) and stroke is markedly increased.[28][29][30] Other possible complications that may arise include: pericarditis, endocarditis, left ventricular failure, valvulitis and fibrosis.[31] Many people with RA do not experience the same chest pain that others feel when they have angina or myocardial infarction. To reduce cardiovascular risk, it is crucial to maintain optimal control of the inflammation caused by RA (which may be involved in causing the cardiovascular risk), and to use exercise and medications appropriately to reduce other cardiovascular risk factors such as blood lipids and blood pressure. Doctors who treat people with RA should be sensitive to cardiovascular risk when prescribing anti-inflammatory medications, and may want to consider prescribing routine use of low doses of aspirin if the gastrointestinal effects are tolerable.[31]
Blood
[edit]Anemia is by far the most common abnormality of the blood cells which can be caused by a variety of mechanisms. The chronic inflammation caused by RA leads to raised hepcidin levels, leading to anemia of chronic disease where iron is poorly absorbed and also sequestered into macrophages. The red cells are of normal size and color (normocytic and Normochromic).[32]
A low white blood cell count usually only occurs in people with Felty's syndrome with an enlarged liver and spleen. The mechanism of neutropenia is complex. An increased platelet count occurs when inflammation is uncontrolled.[33]
Other
[edit]The role of the circadian clock in rheumatoid arthritis suggests a correlation between an early morning rise in circulating levels of pro-inflammatory cytokines, such as interleukin-6 and painful morning joint stiffness.[34]
Kidneys
[edit]Renal amyloidosis can occur as a consequence of untreated chronic inflammation.[35] Treatment with penicillamine or gold salts such as sodium aurothiomalate are recognized causes of membranous nephropathy.[36]
Eyes
[edit]The eye can be directly affected in the form of episcleritis[37] or scleritis, which when severe can very rarely progress to perforating scleromalacia. Rather more common is the indirect effect of keratoconjunctivitis sicca, which is a dryness of eyes and mouth caused by lymphocyte infiltration of lacrimal and salivary glands. When severe, dryness of the cornea can lead to keratitis and loss of vision as well as being painful. Preventive treatment of severe dryness with measures such as nasolacrimal duct blockage is important.[38]
Liver
[edit]Liver problems in people with rheumatoid arthritis may be due to the underlying disease process or as a result of the medications used to treat the disease.[39] A coexisting autoimmune liver disease, such as primary biliary cirrhosis or autoimmune hepatitis may also cause problems.[39]
Neurological
[edit]Peripheral neuropathy and mononeuritis multiplex may occur. The most common problem is carpal tunnel syndrome caused by compression of the median nerve by swelling around the wrist. Rheumatoid disease of the spine can lead to myelopathy. Atlanto-axial subluxation can occur, owing to erosion of the odontoid process and/or transverse ligaments in the cervical spine's connection to the skull. Such an erosion (>3mm) can give rise to vertebrae slipping over one another and compressing the spinal cord. Clumsiness is initially experienced, but without due care, this can progress to quadriplegia or even death.[40]
Constitutional symptoms
[edit]Constitutional symptoms including fatigue, low grade fever, malaise, morning stiffness, loss of appetite and loss of weight are common systemic manifestations seen in people with active RA.
Bones
[edit]Local osteoporosis occurs in RA around inflamed joints. It is postulated to be partially caused by inflammatory cytokines. More general osteoporosis is probably contributed to by immobility, systemic cytokine effects, local cytokine release in bone marrow and corticosteroid therapy.[41][42]
Cancer
[edit]The incidence of lymphoma is increased, although it is uncommon and associated with the chronic inflammation, not the treatment of RA.[43][44] The risk of non-melanoma skin cancer is increased in people with RA compared to the general population, an association possibly due to the use of immunosuppression agents for treating RA.[45]
Teeth
[edit]Periodontitis and tooth loss are common in people with rheumatoid arthritis.[46]
Risk factors
[edit]RA is a systemic (whole body) autoimmune disease. Some genetic and environmental factors affect the risk for RA.
Genetic
[edit]Worldwide, RA affects approximately 1% of the adult population and occurs one in 1,000 children. Studies show RA primarily affects individuals between the ages of 40–60 years and is seen more commonly in females.[47][48] A family history of RA increases the risk around three to five times; as of 2016, it was estimated that genetics may account for 40–65% of cases of seropositive RA, but only around 20% for seronegative RA.[3] RA is strongly associated with genes of the inherited tissue type major histocompatibility complex (MHC) antigen. HLA-DR4 is the major genetic factor implicated – the relative importance varies across ethnic groups.[49]
Genome-wide association studies examining single-nucleotide polymorphisms have found around one hundred alleles associated with RA risk.[50] Risk alleles within the HLA (particularly HLA-DRB1) genes harbor more risk than other loci.[51] The HLA encodes proteins that control recognition of self- versus non-self molecules. Other risk loci include genes affecting co-stimulatory immune pathways—for example CD28 and CD40, cytokine signaling, lymphocyte receptor activation threshold (e.g., PTPN22), and innate immune activation—appear to have less influence than HLA mutations.[3][52]
Environmental
[edit]There are established epigenetic and environmental risk factors for RA.[53][3] Smoking is an established risk factor for RA in Caucasian populations, increasing the risk three times compared to non-smokers, particularly in men, heavy smokers, and those who are rheumatoid factor positive.[54] Modest alcohol consumption may be protective.[55]
Silica exposure has been linked to RA.[56]
Negative findings
[edit]No infectious agent has been consistently linked with RA and there is no evidence of disease clustering to indicate its infectious cause,[49] but periodontal disease has been consistently associated with RA.[3]
The many negative findings suggest that either the trigger varies, or that it might, in fact, be a chance event inherent with the immune response.[57]
Pathophysiology
[edit]RA primarily starts as a state of persistent cellular activation leading to autoimmunity and immune complexes in joints and other organs where it manifests.[58]
The clinical manifestations of disease are primarily inflammation of the synovial membrane and joint damage, and the fibroblast-like synoviocytes play a key role in these pathogenic processes.[17] Three phases of progression of RA are an initiation phase (due to non-specific inflammation), an amplification phase (due to T cell activation), and chronic inflammatory phase, with tissue injury resulting from the cytokines, IL–1, TNF-alpha, and IL–6.[20]
Non-specific inflammation
[edit]Factors allowing an abnormal immune response, once initiated, become permanent and chronic. These factors are genetic disorders which change regulation of the adaptive immune response.[3] Genetic factors interact with environmental risk factors for RA, with cigarette smoking as the most clearly defined risk factor.[54][59]
Other environmental and hormonal factors may explain higher risks for women, including onset after childbirth and hormonal medications. A possibility for increased susceptibility is that negative feedback mechanisms – which normally maintain tolerance – are overtaken by positive feedback mechanisms for certain antigens, such as IgG Fc bound by rheumatoid factor and citrullinated fibrinogen bound by antibodies to citrullinated peptides (ACPA – Anti–citrullinated protein antibody). A debate on the relative roles of B-cell produced immune complexes and T cell products in inflammation in RA has continued for 30 years, but neither cell is necessary at the site of inflammation, only autoantibodies to IgGFc, known as rheumatoid factors and ACPA, with ACPA having an 80% specificity for diagnosing RA.[60] As with other autoimmune diseases, people with RA have abnormally glycosylated antibodies, which are believed to promote joint inflammation.[61]: 10
Amplification in the synovium
[edit]Once the generalized abnormal immune response has become established – which may take several years before any symptoms occur – plasma cells derived from B lymphocytes produce rheumatoid factors and ACPA of the IgG and IgM classes in large quantities. These activate macrophages through Fc receptor and complement binding, which is part of the intense inflammation in RA.[62] Binding of an autoreactive antibody to the Fc receptors is mediated through the antibody's N-glycans, which are altered to promote inflammation in people with RA.[61]: 8
This contributes to local inflammation in a joint, specifically the synovium with edema, vasodilation and entry of activated T-cells, mainly CD4 in microscopically nodular aggregates and CD8 in microscopically diffuse infiltrates.[63]
Synovial macrophages and dendritic cells function as antigen-presenting cells by expressing MHC class II molecules, which establishes the immune reaction in the tissue.[63]
Chronic inflammation
[edit]The disease progresses by forming granulation tissue at the edges of the synovial lining, pannus with extensive angiogenesis and enzymes causing tissue damage.[64] The fibroblast-like synoviocytes have a prominent role in these pathogenic processes.[17] The synovium thickens, cartilage and underlying bone disintegrate, and the joint deteriorates, with raised calprotectin levels serving as a biomarker of these events.[65] Importantly inflammatory events are not limited to synovium but it appear to be systemic, evidence suggest that alterations in T helper profile favoring inflammation such as inflammatory IL-17A producing T helper cells and pathogenic Th17 cells are come from both memory and effector compartment in RA patients peripheral blood.[66]
Cytokines and chemokines attract and accumulate immune cells, i.e. activated T- and B cells, monocytes and macrophages from activated fibroblast-like synoviocytes, in the joint space. By signalling through RANKL and RANK, they eventually trigger osteoclast production, which degrades bone tissue.[3][67][page needed] The fibroblast-like synoviocytes that are present in the synovium during rheumatoid arthritis display altered phenotype compared to the cells present in normal tissues. The aggressive phenotype of fibroblast-like synoviocytes in rheumatoid arthritis and the effect these cells have on the microenvironment of the joint can be summarized into hallmarks that distinguish them from healthy fibroblast-like synoviocytes. These hallmark features of fibroblast-like synoviocytes in rheumatoid arthritis are divided into seven cell-intrinsic hallmarks and four cell-extrinsic hallmarks.[17] The cell-intrinsic hallmarks are: reduced apoptosis, impaired contact inhibition, increased migratory invasive potential, changed epigenetic landscape, temporal and spatial heterogeneity, genomic instability and mutations, and reprogrammed cellular metabolism. The cell-extrinsic hallmarks of FLS in RA are: promotes osteoclastogenesis and bone erosion, contributes to cartilage degradation, induces synovial angiogenesis, and recruits and stimulates immune cells.[17]
Diagnosis
[edit]Imaging
[edit]

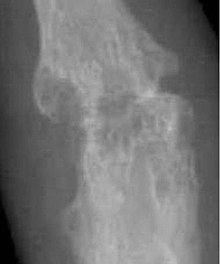
X-rays of the hands and feet are generally performed when many joints affected. In RA, there may be no changes in the early stages of the disease or the x-ray may show osteopenia near the joint, soft tissue swelling, and a smaller than normal joint space. As the disease advances, there may be bony erosions and subluxation. Other medical imaging techniques such as magnetic resonance imaging (MRI) and ultrasound are also used in RA.[20][69]
Technical advances in ultrasonography like high-frequency transducers (10 MHz or higher) have improved the spatial resolution of ultrasound images depicting 20% more erosions than conventional radiography. Color Doppler and power Doppler ultrasound are useful in assessing the degree of synovial inflammation as they can show vascular signals of active synovitis. This is important, since in the early stages of RA, the synovium is primarily affected, and synovitis seems to be the best predictive marker of future joint damage.[70]
Blood tests
[edit]When RA is clinically suspected, a physician may test for rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs measured as anti-CCP antibodies).[71]: 382 The test is positive approximately two-thirds of the time, but a negative RF or CCP antibody does not rule out RA; rather, the arthritis is called seronegative, which occurs in approximately a third of people with RA.[72] During the first year of illness, rheumatoid factor is more likely to be negative with some individuals becoming seropositive over time. RF is a non-specific antibody and seen in about 10% of healthy people, in many other chronic infections like hepatitis C, and chronic autoimmune diseases such as Sjögren's syndrome and systemic lupus erythematosus. Therefore, the test is not specific for RA.[20]
Hence, new serological tests check for anti-citrullinated protein antibodies ACPAs. These tests are again positive in 61–75% of all RA cases, but with a specificity of around 95%.[73] As with RF, ACPAs are many times present before symptoms have started.[20]
The by far most common clinical test for ACPAs is the anti-cyclic citrullinated peptide (anti CCP) ELISA. In 2008 a serological point-of-care test for the early detection of RA combined the detection of RF and anti-MCV with a sensitivity of 72% and specificity of 99.7%.[74][better source needed][75]
To improve the diagnostic capture rate in the early detection of patients with RA and to risk stratify these individuals, the rheumatology field continues to seek complementary markers to both RF and anti-CCP. 14-3-3η (YWHAH) is one such marker that complements RF and anti-CCP, along with other serological measures like C-reactive protein. In a systematic review, 14-3-3η has been described as a welcome addition to the rheumatology field. The authors indicate that the serum based 14-3-η marker is additive to the armamentarium of existing tools available to clinicians, and that there is adequate clinical evidence to support its clinical benefits.[76]
Other blood tests are usually done to differentiate from other causes of arthritis, like the erythrocyte sedimentation rate (ESR), C-reactive protein, full blood count, kidney function, liver enzymes and other immunological tests (e.g., antinuclear antibody/ANA) are all performed at this stage. Elevated ferritin levels can reveal hemochromatosis, a mimic of RA, or be a sign of Still's disease, a seronegative, usually juvenile, variant of rheumatoid Arthritis.[77]
Classification criteria
[edit]In 2010, the 2010 ACR / EULAR Rheumatoid Arthritis Classification Criteria were introduced.[78]
The new criteria are not diagnostic criteria, but are classification criteria to identify disease with a high likelihood of developing a chronic form.[20] However a score of 6 or greater unequivocally classifies a person with a diagnosis of rheumatoid arthritis.[79][citation needed]
These new classification criteria overruled the "old" ACR criteria of 1987 and are adapted for early RA diagnosis. The "new" classification criteria, jointly published by the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) establish a point value between 0 and 10. Four areas are covered in the diagnosis:[78]
- joint involvement, designating the metacarpophalangeal joints, proximal interphalangeal joints, the interphalangeal joint of the thumb, second through fifth metatarsophalangeal joint and wrist as small joints, and shoulders, elbows, hip joints, knees, and ankles as large joints:
- Involvement of 1 large joint gives 0 points
- Involvement of 2–10 large joints gives 1 point
- Involvement of 1–3 small joints (with or without involvement of large joints) gives 2 points
- Involvement of 4–10 small joints (with or without involvement of large joints) gives 3 points
- Involvement of more than 10 joints (with involvement of at least 1 small joint) gives 5 points
- serological parameters – including the rheumatoid factor as well as ACPA – "ACPA" stands for "anti-citrullinated protein antibody":
- Negative RF and negative ACPA gives 0 points
- Low-positive RF or low-positive ACPA gives 2 points
- High-positive RF or high-positive ACPA gives 3 points
- acute phase reactants: 1 point for elevated erythrocyte sedimentation rate, ESR, or elevated CRP value (c-reactive protein)
- duration of arthritis: 1 point for symptoms lasting six weeks or longer
The new criteria accommodate to the growing understanding of RA and the improvements in diagnosing RA and disease treatment. In the "new" criteria, serology and autoimmune diagnostics carries major weight, as ACPA detection is appropriate to diagnose the disease in an early state, before joints destructions occur. Destruction of the joints viewed in radiological images was a significant point of the ACR criteria from 1987.[80] This criterion no longer is regarded to be relevant, as this is just the type of damage that treatment is meant to avoid.
Differential diagnoses
[edit]| Type | WBC (per mm3) | % neutrophils | Viscosity | Appearance |
|---|---|---|---|---|
| Normal | <200 | 0 | High | Transparent |
| Osteoarthritis | <5000 | <25 | High | Clear yellow |
| Trauma | <10,000 | <50 | Variable | Bloody |
| Inflammatory | 2,000–50,000 | 50–80 | Low | Cloudy yellow |
| Septic arthritis | >50,000 | >75 | Low | Cloudy yellow |
| Gonorrhea | ~10,000 | 60 | Low | Cloudy yellow |
| Tuberculosis | ~20,000 | 70 | Low | Cloudy yellow |
| Inflammatory: Arthritis, gout, rheumatoid arthritis, rheumatic fever | ||||
Several other medical conditions can resemble RA, and need to be distinguished from it at the time of diagnosis:[83]
- Crystal induced arthritis (gout, and pseudogout) – usually involves particular joints (knee, MTP1, heels) and can be distinguished with an aspiration of joint fluid if in doubt. Redness, asymmetric distribution of affected joints, pain occurs at night and the starting pain is less than an hour with gout.
- Osteoarthritis – distinguished with X-rays of the affected joints and blood tests, older age, starting pain less than an hour, asymmetric distribution of affected joints and pain worsens when using joint for longer periods.
- Systemic lupus erythematosus (SLE) – distinguished by specific clinical symptoms and blood tests (antibodies against double-stranded DNA)
- One of the several types of psoriatic arthritis resembles RA – nail changes and skin symptoms distinguish between them
- Lyme disease causes erosive arthritis and may closely resemble RA – it may be distinguished by blood test in endemic areas
- Reactive arthritis – asymmetrically involves heel, sacroiliac joints and large joints of the leg. It is usually associated with urethritis, conjunctivitis, iritis, painless buccal ulcers, and keratoderma blennorrhagica.
- Axial spondyloarthritis (including ankylosing spondylitis) – this involves the spine, although an RA-like symmetrical small-joint polyarthritis may occur in the context of this condition.
- Hepatitis C – RA-like symmetrical small-joint polyarthritis may occur in the context of this condition. Hepatitis C may also induce rheumatoid factor auto-antibodies.
Rarer causes which usually behave differently but may cause joint pains:[83]
- Sarcoidosis, amyloidosis, and Whipple's disease can also resemble RA.
- Hemochromatosis may cause hand joint arthritis.
- Acute rheumatic fever can be differentiated by a migratory pattern of joint involvement and evidence of antecedent streptococcal infection.
- Bacterial arthritis (such as by Streptococcus) is usually asymmetric, while RA usually involves both sides of the body symmetrically.
- Gonococcal arthritis (a bacterial arthritis) is also initially migratory and can involve tendons around the wrists and ankles.
Sometimes arthritis is in an undifferentiated stage (i.e. none of the above criteria is positive), even if synovitis is witnessed and assessed with ultrasound imaging.
Difficult-to-treat
[edit]Rheumatoid arthritis (D2T RA) is a specific classification RA by the European League against Rheumatism (EULAR).[84]
Signs of illness:
- Persistence of signs and symptoms
- Drug resistance
- Does not respond on two or more biological treatments
- Does not respond on anti-rheumatic drugs with different mechanism of action
Factors contributing to difficult-to-treat disease:
- Genetic risk factors
- Environmental factors (diet, smoking, physical activity)
- Overweight and obese
Genetic factors
[edit]Genetic factors such as HLA-DR1B1,[85] TRAF1, PSORS1C1 and microRNA 146a[86] are associated with difficult to treat rheumatoid arthritis, other gene polymorphisms seem to be correlated with response to biologic modifying anti-rheumatic drugs (bDMARDs). Next one is FOXO3A gene region been reported as associated with worst disorder. The minor allele at FOXO3A summon a differential response of monocytes in RA patients. FOXO3A can provide an increase of pro-inflammatory cytokines, including TNFα. Possible gene polymorphism: STAT4, PTPN2, PSORS1C1 and TRAF3IP2 genes had been correlated with response to TNF inhibitors.[87]
HLA-DR1 and HLA-DRB1 gene
[edit]The HLA-DRB1 gene is part of a family of genes called the human leukocyte antigen (HLA) complex. The HLA complex is the human version of the major histocompatibility complex (MHC). Currently, have been identified at least 2479 different versions of the HLA-DRB1 gene.[88] The presence of HLA-DRB1 alleles seems to predict radiographic damage, which may be partially mediated by ACPA development, and also elevated sera inflammatory levels and high swollen joint count. HLA-DR1 is encoded by the most risk allele HLA-DRB1 which share a conserved 5-aminoacid sequence that is correlated with the development of anti-citrullinated protein antibodies.[89] HLA-DRB1 gene have more strong correlation with disease development. Susceptibility to and outcome for rheumatoid arthritis (RA) may associate with particular HLA-DR alleles, but these alleles vary among ethnic groups and geographic areas.[90]
MicroRNAs
[edit]MicroRNAs are a factor in the development of that type of disease. MicroRNAs usually operate as a negative regulator of the expression of target proteins and their increased concentration after biologic treatment (bDMARDs) or after anti-rheumatic drugs. Level of miRNA before and after anti-TNFa/DMRADs combination therapy are potential novel biomarkers for predicting and monitoring outcome. For instance, some of them were found significantly upregulated by anti-TNFa/DMRADs combination therapy. For example, miRNA-16-5p, miRNA-23-3p, miRNA125b-5p, miRNA-126-3p, miRNA-146a-5p, miRNA-223-3p. Curious fact is that only responder patients showed an increase in those miRNAs after therapy, and paralleled the reduction of TNFα, interleukin (IL)-6, IL-17, rheumatoid factor (RF), and C-reactive protein (CRP).[91]
Monitoring progression
[edit]Many tools can be used to monitor remission in rheumatoid arthritis.
- DAS28: Disease Activity Score of 28 joints (DAS28) is widely used as an indicator of RA disease activity and response to treatment. Joints included are (bilaterally): proximal interphalangeal joints (10 joints), metacarpophalangeal joints (10), wrists (2), elbows (2), shoulders (2) and knees (2). When looking at these joints, both the number of joints with tenderness upon touching (TEN28) and swelling (SW28) are counted. The erythrocyte sedimentation rate (ESR) is measured and the affected person makes a subjective assessment (SA) of disease activity during the preceding 7 days on a scale between 0 and 100, where 0 is "no activity" and 100 is "highest activity possible". With these parameters, DAS28 is calculated as:[92]
From this, the disease activity of the affected person can be classified as follows:[92]
| Current DAS28 |
DAS28 decrease from initial value | |||
|---|---|---|---|---|
| > 1.2 | > 0.6 but ≤ 1.2 | ≤ 0.6 | ||
| ≤ 3.2 | Inactive | Good improvement | Moderate improvement | No improvement |
| > 3.2 but ≤ 5.1 | Moderate | Moderate improvement | Moderate improvement | No improvement |
| > 5.1 | Very active | Moderate improvement | No improvement | No improvement |
It is not always a reliable indicator of treatment effect.[93] One major limitation is that low-grade synovitis may be missed.[94]
- Other: Other tools to monitor remission in rheumatoid arthritis are: ACR-EULAR Provisional Definition of Remission of Rheumatoid arthritis, Simplified Disease Activity Index and Clinical Disease Activity Index.[95] Some scores do not require input from a healthcare professional and allow self-monitoring by the person, like HAQ-DI.[96][page needed]
Management
[edit]There is no cure for RA, but treatments can improve symptoms and slow the progress of the disease. Disease-modifying treatment has the best results when it is started early and aggressively.[97][48] The results of a recent systematic review found that combination therapy with tumor necrosis factor (TNF) and non-TNF biologics plus methotrexate (MTX) resulted in improved disease control, Disease Activity Score (DAS)-defined remission, and functional capacity compared with a single treatment of either methotrexate or a biologic alone.[98]
The goals of treatment are to minimize symptoms such as pain and swelling, to prevent bone deformity (for example, bone erosions visible in X-rays), and to maintain day-to-day functioning.[99] This is primarily addressed with disease-modifying antirheumatic drugs (DMARDs); dosed physical activity; analgesics and physical therapy may be used to help manage pain.[7][5][6] RA should generally be treated with at least one specific anti-rheumatic medication[8] while combination therapies and corticosteroids are common in treatment.[100] The use of benzodiazepines (such as diazepam) to treat the pain is not recommended as it does not appear to help and is associated with risks.[101]
Lifestyle
[edit]Regular exercise is recommended as both safe and useful to maintain muscle strength and overall physical function.[102] Physical activity is beneficial for people with rheumatoid arthritis who experience fatigue,[103] although there was little to no evidence to suggest that exercise may have an impact on physical function in the long term, a study found that carefully dosed exercise has shown significant improvements in patients with RA.[6][104] Physical activity increases the production of synovial fluid, which lubricates the joints and reduces friction.[105] Moderate effects have been found for aerobic exercises and resistance training on cardiovascular fitness and muscle strength in RA. Furthermore, physical activity had no detrimental side effects like increased disease activity in any exercise dimension.[106] It is uncertain if eating or avoiding specific foods or other specific dietary measures help improve symptoms,[107] but several studies have shown that high-vegetable diets improve RA symptoms whereas high-meat diets make symptoms worse. [1] Occupational therapy has a positive role to play in improving functional ability in people with rheumatoid arthritis.[108] Weak evidence supports the use of wax baths (thermotherapy) to treat arthritis in the hands.[109]
Educational approaches that inform people about tools and strategies available to help them cope with rheumatoid arthritis may improve a person's psychological status and level of depression in the shorter-term.[110] The use of extra-depth shoes and molded insoles may reduce pain during weight-bearing activities such as walking.[111] Insoles may also prevent the progression of bunions.[111]
Disease-modifying agents
[edit]Disease-modifying antirheumatic drugs (DMARDs) are the primary treatment for RA.[8] They are a diverse collection of drugs, grouped by use and convention. They have been found to improve symptoms, decrease joint damage, and improve overall functional abilities.[8] DMARDs should be started early in the disease as they result in disease remission in approximately half of people and improved outcomes overall.[8]
The following drugs are considered DMARDs: methotrexate, sulfasalazine, leflunomide, hydroxychloroquine, TNF inhibitors (certolizumab, adalimumab, infliximab and etanercept), abatacept, anakinra, and auranofin. Additionally, rituximab and tocilizumab are monoclonal antibodies and are also DMARDs.[8] Use of tocilizumab is associated with a risk of increased cholesterol levels.[112]
The most commonly used agent is methotrexate with other frequently used agents including sulfasalazine and leflunomide.[8] Leflunomide is effective when used from 6–12 months, with similar effectiveness to methotrexate when used for 2 years.[113] Sulfasalazine also appears to be most effective in the short-term treatment of rheumatoid arthritis.[114]
Hydroxychloroquine, in addition to its low toxicity profile, is considered effective for treatment of moderate RA symptoms.[115]
Agents may be used in combination, however, people may experience greater side effects.[8][116] Methotrexate is the most important and useful DMARD and is usually the first treatment.[8][5][117] A combined approach with methotrexate and biologics improves ACR50, HAQ scores and RA remission rates.[118][48] This benefit from the combination of methotrexate with biologics occurs both when this combination is the initial treatment and when drugs are prescribed in a sequential or step-up manner.[48] Triple therapy consisting of methotrexate, sulfasalazine and hydroxychloroquine may also effectively control disease activity.[119] Adverse effects should be monitored regularly with toxicity including gastrointestinal, hematologic, pulmonary, and hepatic.[117] Side effects such as nausea, vomiting or abdominal pain can be reduced by taking folic acid.[120]
Rituximab combined with methotrexate appears to be more effective in improving symptoms compared to methotrexate alone.[121] Rituximab works by decreasing levels of B-cells (immune cell that is involved in inflammation). People taking rituximab had improved pain, function, reduced disease activity and reduced joint damage based on x-ray images. After 6 months, 21% more people had improvement in their symptoms using rituximab and methotrexate.[121]
Biological agents should generally be used only if methotrexate and other conventional agents are not effective after a trial of three months.[8] They are associated with a higher rate of serious infections as compared to other DMARDs.[122] Biological DMARD agents used to treat rheumatoid arthritis include: tumor necrosis factor alpha inhibitors (TNF inhibitors) such as infliximab; interleukin 1 blockers such as anakinra, monoclonal antibodies against B cells such as rituximab, interleukin 6 blockers such as tocilizumab, and T cell co-stimulation blockers such as abatacept. They are often used in combination with either methotrexate or leflunomide.[8][3] Biologic monotherapy or tofacitinib with methotrexate may improve ACR50, RA remission rates and function.[123][124] Abatacept should not be used at the same time as other biologics.[125] In those who are well controlled (low disease activity) on TNF inhibitors, decreasing the dose does not appear to affect overall function.[126] Discontinuation of TNF inhibitors (as opposed to gradually lowering the dose) by people with low disease activity may lead to increased disease activity and may affect remission, damage that is visible on an x-ray, and a person's function.[126] People should be screened for latent tuberculosis before starting any TNF inhibitor therapy to avoid reactivation of tuberculosis.[20]
TNF inhibitors and methotrexate appear to have similar effectiveness when used alone and better results are obtained when used together.[127] Golimumab is effective when used with methotraxate.[128] TNF inhibitors may have equivalent effectiveness with etanercept appearing to be the safest.[129] Injecting etanercept, in addition to methotrexate twice a week may improve ACR50 and decrease radiographic progression for up to 3 years.[130] Abatacept appears effective for RA with 20% more people improving with treatment than without but long term safety studies are yet unavailable.[131] Adalimumab slows the time for the radiographic progression when used for 52 weeks.[132] However, there is a lack of evidence to distinguish between the biologics available for RA.[133] Issues with the biologics include their high cost and association with infections including tuberculosis.[3] Use of biological agents may reduce fatigue.[134] The mechanism of how biologics reduce fatigue is unclear.[134]
Gold and cyclosporin
[edit]Sodium aurothiomalate, auranofin, and cyclosporin are less commonly used due to more common adverse effects.[8] However, cyclosporin was found to be effective in the progressive RA when used up to one year.[135]
Anti-inflammatory and analgesic agents
[edit]Glucocorticoids can be used in the short term and at the lowest dose possible for flare-ups and while waiting for slow-onset drugs to take effect.[8][3][136] Combination of glucocorticoids and conventional therapy has shown a decrease in rate of erosion of bones.[137] Steroids may be injected into affected joints during the initial period of RA, prior to the use of DMARDs or oral steroids.[138]
Non-NSAID drugs to relieve pain, like paracetamol may be used to help relieve the pain symptoms; they do not change the underlying disease.[5] The use of paracetamol may be associated with the risk of developing ulcers.[139]
NSAIDs reduce both pain and stiffness in those with RA but do not affect the underlying disease and appear to have no effect on people's long term disease course and thus are no longer first line agents.[3][140] NSAIDs should be used with caution in those with gastrointestinal, cardiovascular, or kidney problems.[141][142][143][139] Rofecoxib was withdrawn from the global market as its long-term use was associated to an increased risk of heart attacks and strokes.[144] Use of methotrexate together with NSAIDs is safe, if adequate monitoring is done.[145] COX-2 inhibitors, such as celecoxib, and NSAIDs are equally effective.[146][147] A 2004 Cochrane review found that people preferred NSAIDs over paracetamol.[148] However, it is yet to be clinically determined whether NSAIDs are more effective than paracetamol.[148]
The neuromodulator agents topical capsaicin may be reasonable to use in an attempt to reduce pain.[149] Nefopam by mouth and cannabis are not recommended as of 2012 as the risks of use appear to be greater than the benefits.[149]
Limited evidence suggests the use of weak oral opioids but the adverse effects may outweigh the benefits.[150]
Alternatively, physical therapy has been tested and shown as an effective aid in reducing pain in patients with RA. As most RA is detected early and treated aggressively, physical therapy plays more of a preventative and compensatory role, aiding in pain management alongside regular rheumatic therapy.[7]
Surgery
[edit]Especially for affected fingers, hands, and wrists, synovectomy may be needed to prevent pain or tendon rupture when drug treatment has failed. Severely affected joints may require joint replacement surgery, such as knee replacement. Postoperatively, physiotherapy is always necessary.[16]: 1080, 1103 There is insufficient evidence to support surgical treatment on arthritic shoulders.[151]
Physiotherapy
[edit]For people with RA, physiotherapy may be used together with medical management.[152] This may include cold and heat application, electronic stimulation, and hydrotherapy.[152] Although medications improve symptoms of RA, muscle function is not regained when disease activity is controlled.[153]
Physiotherapy promotes physical activity. In RA, physical activity like exercise in the appropriate dosage (frequency, intensity, time, type, volume, progression) and physical activity promotion is effective in improving cardiovascular fitness, muscle strength, and maintaining a long term active lifestyle. In the short term, resistance exercises, with or without range of motion exercises, improve self-reported hand functions.[153] Physical activity promotion according to the public health recommendations should be an integral part of standard care for people with RA and other arthritic diseases.[6] Additionally, the combination of physical activities and cryotherapy show its efficacy on the disease activity and pain relief.[154] The combination of aerobic activity and cryotherapy may be an innovative therapeutic strategy to improve the aerobic capacity in arthritis patients and consequently reduce their cardiovascular risk while minimizing pain and disease activity.[154]
Compression gloves
[edit]Compression gloves are handwear designed to help prevent the occurrence of various medical disorders relating to blood circulation in the wrists and hands. They can be used to treat the symptoms of arthritis,[155] though the medical benefits may be limited.[156]
Alternative medicine
[edit]In general, there is not enough evidence to support any complementary health approaches for RA, with safety concerns for some of them. Some mind and body practices and dietary supplements may help people with symptoms and therefore may be beneficial additions to conventional treatments, but there is not enough evidence to draw conclusions.[157] A systematic review of CAM modalities (excluding fish oil) found that " The available evidence does not support their current use in the management of RA."[158] Studies showing beneficial effects in RA on a wide variety of CAM modalities are often affected by publication bias and are generally not high quality evidence such as randomized controlled trials (RCTs).[159]
A 2005 Cochrane review states that low level laser therapy can be tried to improve pain and morning stiffness due to rheumatoid arthritis as there are few side-effects.[160]
There is limited evidence that tai chi might improve the range of motion of a joint in persons with rheumatoid arthritis.[161][162] The evidence for acupuncture is inconclusive[163] with it appearing to be equivalent to sham acupuncture.[164]
A Cochrane review in 2002 showed some benefits of the electrical stimulation as a rehabilitation intervention to improve the power of the hand grip and help to resist fatigue.[165] D‐penicillamine may provide similar benefits as DMARDs but it is also highly toxic.[166] Low-quality evidence suggests the use of therapeutic ultrasound on arthritic hands.[167] Potential benefits include increased grip strength, reduced morning stiffness and number of swollen joints.[167] There is tentative evidence of benefit of transcutaneous electrical nerve stimulation (TENS) in RA.[168] Acupuncture‐like TENS (AL-TENS) may decrease pain intensity and improve muscle power scores.[168]
Low-quality evidence suggests people with active RA may benefit from assistive technology.[169] This may include less discomfort and difficulty such as when using an eye drop device.[169] Balance training is of unclear benefits.[170]
Dietary supplements
[edit]Fatty acids
[edit]There has been a growing interest in the role of long-chain omega-3 polyunsaturated fatty acids to reduce inflammation and alleviate the symptoms of RA. Metabolism of omega-3 polyunsaturated fatty acids produces docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), which inhibits pro-inflammatory eicosanoids and cytokines (TNF-a, IL-1b and IL-6), decreasing both lymphocyte proliferation and reactive oxygen species.[171][172] These studies showed evidence for significant clinical improvements on RA in inflammatory status and articular index. Gamma-linolenic acid, an omega-6 fatty acid, may reduce pain, tender joint count and stiffness, and is generally safe.[173] For omega-3 polyunsaturated fatty acids (found in fish oil, flax oil and hemp oil), a meta-analysis reported a favorable effect on pain, although confidence in the effect was considered moderate. The same review reported less inflammation but no difference in joint function.[174] A review examined the effect of marine oil omega-3 fatty acids on pro-inflammatory eicosanoid concentrations; leukotriene4 (LTB4) was lowered in people with rheumatoid arthritis but not in those with non-autoimmune chronic diseases.[175] Fish consumption has no association with RA.[176] A fourth review limited inclusion to trials in which people eat ≥2.7 g/day for more than three months. Use of pain relief medication was decreased, but improvements in tender or swollen joints, morning stiffness and physical function were not changed.[177] Collectively, the current evidence is not strong enough to determine that supplementation with omega-3 fatty acids or regular consumption of fish are effective treatments for rheumatoid arthritis.[174][175][176][177]
Herbal
[edit]The American College of Rheumatology states that no herbal medicines have health claims supported by high-quality evidence and thus they do not recommend their use.[178] There is no scientific basis to suggest that herbal supplements advertised as "natural" are safer for use than conventional medications as both are chemicals. Herbal medications, although labelled "natural", may be toxic or fatal if consumed.[178] Due to the false belief that herbal supplements are always safe, there is sometimes a hesitancy to report their use which may increase the risk of adverse reactions.[159]
Pregnancy
[edit]More than 75% of women with rheumatoid arthritis have symptoms improve during pregnancy but might have symptoms worsen after delivery.[20] Methotrexate and leflunomide are teratogenic (harmful to foetus) and not used in pregnancy. It is recommended women of childbearing age should use contraceptives to avoid pregnancy and to discontinue its use if pregnancy is planned.[99][117] Low dose of prednisolone, hydroxychloroquine and sulfasalazine are considered safe in pregnant women with rheumatoid arthritis. Prednisolone should be used with caution as the side effects include infections and fractures.[179]
Vaccinations
[edit]People with RA have an increased risk of infections and mortality and recommended vaccinations can reduce these risks.[180] The inactivated influenza vaccine should be received annually.[181] The pneumococcal vaccine should be administered twice for people under the age 65 and once for those over 65.[182] Lastly, the live-attenuated zoster vaccine should be administered once after the age 60, but is not recommended in people on a tumor necrosis factor alpha blocker.[183]
Prognosis
[edit]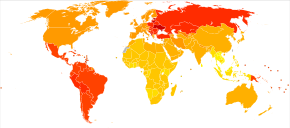
The course of the disease varies greatly. Some people have mild short-term symptoms, but in most the disease is progressive for life. Around 25% will have subcutaneous nodules (known as rheumatoid nodules);[185] this is associated with a poor prognosis.[186]
Prognostic factors
[edit]Poor prognostic factors include,
- Persistent synovitis
- Early erosive disease
- Extra-articular findings (including subcutaneous rheumatoid nodules)
- Positive serum RF findings
- Positive serum anti-CCP autoantibodies
- Positive serum 14-3-3η (YWHAH) levels above 0.5 ng/ml [187][188]
- Carriership of HLA-DR4 "Shared Epitope" alleles
- Family history of RA
- Poor functional status
- Socioeconomic factors[48]
- Elevated acute phase response (erythrocyte sedimentation rate [ESR], C-reactive protein [CRP])
- Increased clinical severity.
- Distance from primary care and specialist care in rural communities[48]
Mortality
[edit]RA reduces lifespan on average from three to twelve years.[99] Young age at onset, long disease duration, the presence of other health problems, and characteristics of severe RA – such as poor functional ability or overall health status, a lot of joint damage on x-rays, the need for hospitalisation or involvement of organs other than the joints – have been shown to associate with higher mortality.[189] Positive responses to treatment may indicate a better prognosis. A 2005 study by the Mayo Clinic noted that individuals with RA have a doubled risk of heart disease,[190] independent of other risk factors such as diabetes, excessive alcohol use, and elevated cholesterol, blood pressure and body mass index. The mechanism by which RA causes this increased risk remains unknown; the presence of chronic inflammation has been proposed as a contributing factor.[191] It is possible that the use of new biologic drug therapies extend the lifespan of people with RA and reduce the risk and progression of atherosclerosis.[192] This is based on cohort and registry studies, and still remains hypothetical. It is still uncertain whether biologics improve vascular function in RA or not. There was an increase in total cholesterol and HDLc levels and no improvement of the atherogenic index.[193]
Epidemiology
[edit]
RA affects 0.5–1% of adults in the developed world with between 5 and 50 per 100,000 people newly developing the condition each year.[3] In 2010 it resulted in about 49,000 deaths globally.[194]
Onset is uncommon under the age of 15 and from then on the incidence rises with age until the age of 80. Women are affected three to five times as often as men.[20]
The age at which the disease most commonly starts is in women between 40 and 50 years of age, and for men somewhat later.[195] RA is a chronic disease,[196] and although rarely, a spontaneous remission may occur,[197] the common course of progression consists of persistent symptoms that wax and wane in intensity, along with continued deterioration of joint structures, leading to deformation and disability.[198][199]
There is an association between periodontitis and rheumatoid arthritis (RA), hypothesised to lead to enhanced generation of RA-related autoantibodies. Oral bacteria that invade the blood may also contribute to chronic inflammatory responses and generation of autoantibodies.[200]
History
[edit]The first recognized description of RA in modern medicine was in 1800 by the French physician Augustin Jacob Landré-Beauvais (1772–1840) who was based in the famed Salpêtrière Hospital in Paris.[12] The name "rheumatoid arthritis" itself was coined in 1859 by British rheumatologist Alfred Baring Garrod.[201]
The art of Peter Paul Rubens may possibly depict the effects of RA. In his later paintings, his rendered hands show, in the opinion of some physicians, increasing deformity consistent with the symptoms of the disease.[202][203] RA appears to some to have been depicted in 16th-century paintings.[204] However, it is generally recognized in art historical circles that the painting of hands in the 16th and 17th century followed certain stylized conventions, most clearly seen in the Mannerist movement. It was conventional, for instance, to show the upheld right hand of Christ in what now appears a deformed posture. These conventions are easily misinterpreted as portrayals of disease.[citation needed]
Historic (though not necessarily effective) treatments for RA have also included: rest, ice, compression and elevation, apple diet, nutmeg, some light exercise every now and then, nettles, bee venom, copper bracelets, rhubarb diet, extractions of teeth, fasting, honey, vitamins, insulin, magnets, and electroconvulsive therapy (ECT).[205]
Etymology
[edit]Rheumatoid arthritis is derived from the Greek word ῥεύμα-rheuma (nom.), ῥεύματος-rheumatos (gen.) ("flow, current"). The suffix -oid ("resembling") gives the translation as joint inflammation that resembles rheumatic fever. Rhuma which means watery discharge might refer to the fact that the joints are swollen or that the disease may be made worse by wet weather.[13]
Research
[edit]Meta-analysis found an association between periodontal disease and RA, but the mechanism of this association remains unclear.[206] Two bacterial species associated with periodontitis are implicated as mediators of protein citrullination in the gums of people with RA.[3]
Vitamin D deficiency is more common in people with rheumatoid arthritis than in the general population.[207][208] However, whether vitamin D deficiency is a cause or a consequence of the disease remains unclear.[209] One meta-analysis found that vitamin D levels are low in people with rheumatoid arthritis and that vitamin D status correlates inversely with prevalence of rheumatoid arthritis, suggesting that vitamin D deficiency is associated with susceptibility to rheumatoid arthritis.[210]
The fibroblast-like synoviocytes have a prominent role in the pathogenic processes of the rheumatic joints, and therapies that target these cells are emerging as promising therapeutic tools, raising hope for future applications in rheumatoid arthritis.[17]
Possible links with intestinal barrier dysfunction are investigated.[211]
See also
[edit]References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t u v w x "Handout on Health: Rheumatoid Arthritis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. August 2014. Archived from the original on June 30, 2015. Retrieved July 2, 2015.
- ^ a b c d e f Majithia V, Geraci SA (November 2007). "Rheumatoid arthritis: diagnosis and management". The American Journal of Medicine. 120 (11): 936–939. doi:10.1016/j.amjmed.2007.04.005. PMID 17976416.
- ^ a b c d e f g h i j k l m n Smolen JS, Aletaha D, McInnes IB (October 2016). "Rheumatoid arthritis" (PDF). Lancet. 388 (10055): 2023–2038. doi:10.1016/S0140-6736(16)30173-8. PMID 27156434. S2CID 37973054.
- ^ Wang H, Naghavi M, Allen C, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ a b c d "Rheumatoid arthritis in adults: management: recommendations: Guidance and guidelines". NICE. December 2015. Archived from the original on 2017-04-16.
- ^ a b c d Rausch Osthoff AK, Juhl CB, Knittle K, et al. (2018-12-04). "Effects of exercise and physical activity promotion: meta-analysis informing the 2018 EULAR recommendations for physical activity in people with rheumatoid arthritis, spondyloarthritis and hip/knee osteoarthritis". RMD Open. 4 (2): e000713. doi:10.1136/rmdopen-2018-000713. PMC 6307596. PMID 30622734.
- ^ a b c Park Y, Chang M (January 2016). "Effects of rehabilitation for pain relief in patients with rheumatoid arthritis: a systematic review". Journal of Physical Therapy Science. 28 (1): 304–308. doi:10.1589/jpts.28.304. PMC 4756025. PMID 26957779.
- ^ a b c d e f g h i j k l m Singh JA, Saag KG, Bridges SL, et al. (January 2016). "2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis". Arthritis & Rheumatology. 68 (1): 1–26. doi:10.1002/art.39480. PMID 26545940. S2CID 42638848.
- ^ Singh JA, Wells GA, Christensen R, et al. (February 2011). "Adverse effects of biologics: a network meta-analysis and Cochrane overview". The Cochrane Database of Systematic Reviews. 2011 (2): CD008794. doi:10.1002/14651858.CD008794.pub2. PMC 7173749. PMID 21328309.
- ^ Vos T, Allen C, Arora M, et al. (GBD 2015 Disease and Injury Incidence and Prevalence Collaborators) (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ^ GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–171. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ^ a b Landré-Beauvais AJ (1800). La goutte asthénique primitive (doctoral thesis). Paris. reproduced in Landré-Beauvais AJ (March 2001). "The first description of rheumatoid arthritis. Unabridged text of the doctoral dissertation presented in 1800". Joint, Bone, Spine. 68 (2): 130–143. doi:10.1016/S1297-319X(00)00247-5. PMID 11324929.
- ^ a b Paget SA, Lockshin MD, Loebl S (2002). The Hospital for Special Surgery Rheumatoid Arthritis Handbook Everything You Need to Know. New York: John Wiley & Sons. p. 32. ISBN 978-0-471-22334-4. Archived from the original on 2017-02-22.
- ^ Turesson C, O'Fallon WM, Crowson CS, et al. (August 2003). "Extra-articular disease manifestations in rheumatoid arthritis: incidence trends and risk factors over 46 years". Annals of the Rheumatic Diseases. 62 (8): 722–727. doi:10.1136/ard.62.8.722. PMC 1754626. PMID 12860726.
- ^ Cutolo M, Kitas GD, van Riel PL (February 2014). "Burden of disease in treated rheumatoid arthritis patients: going beyond the joint". Seminars in Arthritis and Rheumatism. 43 (4): 479–488. doi:10.1016/j.semarthrit.2013.08.004. PMID 24080116.
- ^ a b c d Walker BR, Colledge NR, Ralston SH, Penman ID, eds. (2014). Davidson's principles and practice of medicine (22nd ed.). Churchill Livingstone/Elsevier. ISBN 978-0-7020-5035-0.
- ^ a b c d e f Nygaard G, Firestein GS (June 2020). "Restoring synovial homeostasis in rheumatoid arthritis by targeting fibroblast-like synoviocytes". Nature Reviews. Rheumatology. 16 (6): 316–333. doi:10.1038/s41584-020-0413-5. PMC 7987137. PMID 32393826. S2CID 218573182.
- ^ Suresh E (September 2004). "Diagnosis of early rheumatoid arthritis: what the non-specialist needs to know". Journal of the Royal Society of Medicine. 97 (9): 421–424. doi:10.1177/014107680409700903. PMC 1079582. PMID 15340020.
- ^ Gaffo A, Saag KG, Curtis JR (December 2006). "Treatment of rheumatoid arthritis". American Journal of Health-System Pharmacy. 63 (24): 2451–2465. doi:10.2146/ajhp050514. PMC 5164397. PMID 17158693.
- ^ a b c d e f g h i Shah A (2012). Harrison's Principles of Internal Medicine (18th ed.). United States: McGraw Hill. p. 2738. ISBN 978-0-07-174889-6.
- ^ Turesson C (May 2013). "Extra-articular rheumatoid arthritis". Current Opinion in Rheumatology. 25 (3): 360–366. doi:10.1097/bor.0b013e32835f693f. PMID 23425964. S2CID 21462453.
- ^ Ziff M (June 1990). "The rheumatoid nodule". Arthritis and Rheumatism. 33 (6): 761–767. doi:10.1002/art.1780330601. PMID 2194460.
- ^ Genta MS, Genta RM, Gabay C (October 2006). "Systemic rheumatoid vasculitis: a review". Seminars in Arthritis and Rheumatism. 36 (2): 88–98. doi:10.1016/j.semarthrit.2006.04.006. PMID 17023257.
- ^ Moriyama T. "Chronic Disease". Immunotherapy cancer and chronic disease. Retrieved 2024-05-09.
- ^ a b Khan P, Beigi M (2018). Alopecia Areata. doi:10.1007/978-3-319-72134-7. ISBN 978-3-319-72133-0. S2CID 46954629.
- ^ Kim EJ, Collard HR, King TE (November 2009). "Rheumatoid arthritis-associated interstitial lung disease: the relevance of histopathologic and radiographic pattern". Chest. 136 (5): 1397–1405. doi:10.1378/chest.09-0444. PMC 2818853. PMID 19892679.
- ^ Balbir-Gurman A, Yigla M, Nahir AM, et al. (June 2006). "Rheumatoid pleural effusion". Seminars in Arthritis and Rheumatism. 35 (6): 368–378. doi:10.1016/j.semarthrit.2006.03.002. PMID 16765714.
- ^ Wolfe F, Mitchell DM, Sibley JT, et al. (April 1994). "The mortality of rheumatoid arthritis". Arthritis and Rheumatism. 37 (4): 481–494. doi:10.1002/art.1780370408. PMID 8147925.
- ^ Aviña-Zubieta JA, Choi HK, Sadatsafavi M, et al. (December 2008). "Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies". Arthritis and Rheumatism. 59 (12): 1690–1697. doi:10.1002/art.24092. PMID 19035419.
- ^ Alenghat FJ (February 2016). "The Prevalence of Atherosclerosis in Those with Inflammatory Connective Tissue Disease by Race, Age, and Traditional Risk Factors". Scientific Reports. 6: 20303. Bibcode:2016NatSR...620303A. doi:10.1038/srep20303. PMC 4740809. PMID 26842423.
- ^ a b Gupta A, Fomberstein B (2009). "Evaluating cardiovascular risk in rheumatoid arthritis". Journal of Musculoskeletal Medicine. 26 (8): 481–494. Archived from the original on 2012-07-23.
- ^ Wilson A, Yu HT, Goodnough LT, et al. (April 2004). "Prevalence and outcomes of anemia in rheumatoid arthritis: a systematic review of the literature". The American Journal of Medicine. 116 (Suppl 7A): 50S–57S. doi:10.1016/j.amjmed.2003.12.012. PMID 15050886.
- ^ Tramś E, Malesa K, Pomianowski S, et al. (March 2022). "Role of Platelets in Osteoarthritis-Updated Systematic Review and Meta-Analysis on the Role of Platelet-Rich Plasma in Osteoarthritis". Cells. 11 (7): 1080. doi:10.3390/cells11071080. PMC 8997794. PMID 35406644.
- ^ Gibbs JE, Ray DW (February 2013). "The role of the circadian clock in rheumatoid arthritis". Arthritis Res Ther. 15 (1): 205. doi:10.1186/ar4146. PMC 3672712. PMID 23427807.
- ^ de Groot K (August 2007). "[Renal manifestations in rheumatic diseases]". Der Internist. 48 (8): 779–785. doi:10.1007/s00108-007-1887-9. PMID 17571244. S2CID 28781598.
- ^ Moroni G, Ponticelli C (2020). "Secondary Membranous Nephropathy. A Narrative Review". Frontiers in Medicine. 7: 611317. doi:10.3389/fmed.2020.611317. PMC 7744820. PMID 33344486.
- ^ Schonberg S, Stokkermans TJ (January 2020). "Episcleritis". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30521217.
- ^ Dammacco R, Guerriero S, Alessio G, et al. (February 2022). "Natural and iatrogenic ocular manifestations of rheumatoid arthritis: a systematic review". International Ophthalmology. 42 (2): 689–711. doi:10.1007/s10792-021-02058-8. PMC 8882568. PMID 34802085.
- ^ a b Selmi C, De Santis M, Gershwin ME (June 2011). "Liver involvement in subjects with rheumatic disease". Arthritis Research & Therapy. 13 (3): 226. doi:10.1186/ar3319. PMC 3218873. PMID 21722332.
- ^ Wasserman BR, Moskovich R, Razi AE (2011). "Rheumatoid arthritis of the cervical spine--clinical considerations" (PDF). Bulletin of the NYU Hospital for Joint Diseases. 69 (2): 136–148. PMID 22035393.
- ^ Ginaldi L, Di Benedetto MC, De Martinis M (November 2005). "Osteoporosis, inflammation and ageing". Immunity & Ageing. 2: 14. doi:10.1186/1742-4933-2-14. PMC 1308846. PMID 16271143.
- ^ Ilias I, Milionis C, Zoumakis E (March 2022). "An Overview of Glucocorticoid-Induced Osteoporosis.". In Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, et al. (eds.). Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc. PMID 25905202.
- ^ Baecklund E, Iliadou A, Askling J, et al. (March 2006). "Association of chronic inflammation, not its treatment, with increased lymphoma risk in rheumatoid arthritis". Arthritis and Rheumatism. 54 (3): 692–701. doi:10.1002/art.21675. PMID 16508929.
- ^ Franklin J, Lunt M, Bunn D, et al. (May 2006). "Incidence of lymphoma in a large primary care derived cohort of cases of inflammatory polyarthritis". Annals of the Rheumatic Diseases. 65 (5): 617–622. doi:10.1136/ard.2005.044784. PMC 1798140. PMID 16249224.
- ^ Assassi S (January 2016). "Rheumatoid arthritis, TNF inhibitors, and non-melanoma skin cancer". BMJ. 352: i472. doi:10.1136/bmj.i472. PMID 26822198. S2CID 45857932.
- ^ de Pablo P, Chapple IL, Buckley CD, et al. (April 2009). "Periodontitis in systemic rheumatic diseases". Nature Reviews. Rheumatology. 5 (4): 218–224. doi:10.1038/nrrheum.2009.28. PMID 19337286. S2CID 7173008.
- ^ Rennie KL, Hughes J, Lang R, et al. (April 2003). "Nutritional management of rheumatoid arthritis: a review of the evidence". Journal of Human Nutrition and Dietetics. 16 (2): 97–109. doi:10.1046/j.1365-277x.2003.00423.x. PMID 12662368.
- ^ a b c d e f Donahue KE, Gartlehner G, Schulman ER, et al. (2018). Drug Therapy for Early Rheumatoid Arthritis: A Systematic Review Update. AHRQ Comparative Effectiveness Reviews. Rockville (MD): Agency for Healthcare Research and Quality (US). PMID 30199187.
- ^ a b Doherty M, Lanyon P, Ralston SH. Musculosketal Disorders-Davidson's Principle of Internal Medicine (20th ed.). Elsevier. pp. 1100–1106.
- ^ Okada Y, Wu D, Trynka G, et al. (February 2014). "Genetics of rheumatoid arthritis contributes to biology and drug discovery". Nature. 506 (7488): 376–381. Bibcode:2014Natur.506..376.. doi:10.1038/nature12873. PMC 3944098. PMID 24390342.
- ^ Raychaudhuri S, Sandor C, Stahl EA, et al. (January 2012). "Five amino acids in three HLA proteins explain most of the association between MHC and seropositive rheumatoid arthritis". Nature Genetics. 44 (3): 291–296. doi:10.1038/ng.1076. PMC 3288335. PMID 22286218.
- ^ Ghorban K, Ezzeddini R, Eslami M, et al. (December 2019). "PTPN22 1858 C/T polymorphism is associated with alteration of cytokine profiles as a potential pathogenic mechanism in rheumatoid arthritis". Immunology Letters. 216: 106–113. doi:10.1016/j.imlet.2019.10.010. PMID 31669381. S2CID 204966226.
- ^ Firestein GS, McInnes IB (February 2017). "Immunopathogenesis of Rheumatoid Arthritis". Immunity. 46 (2): 183–196. doi:10.1016/j.immuni.2017.02.006. PMC 5385708. PMID 28228278.(subscription required)
- ^ a b Sugiyama D, Nishimura K, Tamaki K, et al. (January 2010). "Impact of smoking as a risk factor for developing rheumatoid arthritis: a meta-analysis of observational studies" (PDF). Annals of the Rheumatic Diseases. 69 (1): 70–81. doi:10.1136/ard.2008.096487. PMID 19174392. S2CID 11303269. Archived from the original (PDF) on 2021-03-01. Retrieved 2018-04-20.(subscription required)
- ^ Liao KP, Alfredsson L, Karlson EW (May 2009). "Environmental influences on risk for rheumatoid arthritis". Current Opinion in Rheumatology. 21 (3): 279–283. doi:10.1097/BOR.0b013e32832a2e16. PMC 2898190. PMID 19318947.(subscription required)
- ^ Pollard KM (11 March 2016). "Silica, Silicosis, and Autoimmunity". Frontiers in Immunology. 7: 97. doi:10.3389/fimmu.2016.00097. PMC 4786551. PMID 27014276.
- ^ Edwards JC, Cambridge G, Abrahams VM (June 1999). "Do self-perpetuating B lymphocytes drive human autoimmune disease?". Immunology. 97 (2): 188–196. doi:10.1046/j.1365-2567.1999.00772.x. PMC 2326840. PMID 10447731.(subscription required)
- ^ Coates LC, FitzGerald O, Helliwell PS, et al. (December 2016). "Psoriasis, psoriatic arthritis, and rheumatoid arthritis: Is all inflammation the same?". Seminars in Arthritis and Rheumatism. 46 (3): 291–304. doi:10.1016/j.semarthrit.2016.05.012. PMID 27388027. S2CID 22539356.
- ^ Padyukov L, Silva C, Stolt P, et al. (October 2004). "A gene-environment interaction between smoking and shared epitope genes in HLA-DR provides a high risk of seropositive rheumatoid arthritis". Arthritis and Rheumatism. 50 (10): 3085–3092. doi:10.1002/art.20553. PMID 15476204.(subscription required)
- ^ Hua C, Daien CI, Combe B, et al. (2017). "Diagnosis, prognosis and classification of early arthritis: results of a systematic review informing the 2016 update of the EULAR recommendations for the management of early arthritis". RMD Open. 3 (1): e000406. doi:10.1136/rmdopen-2016-000406. PMC 5237764. PMID 28155923.
- ^ a b Maverakis E, Kim K, Shimoda M, et al. (February 2015). "Glycans in the immune system and The Altered Glycan Theory of Autoimmunity: a critical review". Journal of Autoimmunity. 57 (6): 1–13. doi:10.1016/j.jaut.2014.12.002. PMC 4340844. PMID 25578468.(subscription required)
- ^ Boldt AB, Goeldner I, de Messias-Reason IJ (2012). "Relevance of the lectin pathway of complement in rheumatic diseases". In Makowski G (ed.). Advances in Clinical Chemistry. Vol. 56. Elsevier. pp. 105–153. doi:10.1016/B978-0-12-394317-0.00012-1. ISBN 978-0-12-394317-0. PMID 22397030.(subscription required)
- ^ a b Jonsson AH, Zhang F, Dunlap G, et al. (June 2022). "Granzyme K+ CD8 T cells form a core population in inflamed human tissue". Science Translational Medicine. 14 (649): eabo0686. doi:10.1126/scitranslmed.abo0686. PMC 9972878. PMID 35704599.
- ^ Elshabrawy HA, Chen Z, Volin MV, et al. (October 2015). "The pathogenic role of angiogenesis in rheumatoid arthritis". Angiogenesis. 18 (4): 433–448. doi:10.1007/s10456-015-9477-2. PMC 4879881. PMID 26198292.
- ^ Abildtrup M, Kingsley GH, Scott DL (May 2015). "Calprotectin as a biomarker for rheumatoid arthritis: a systematic review". The Journal of Rheumatology. 42 (5): 760–770. doi:10.3899/jrheum.140628. PMID 25729036. S2CID 43537545.
- ^ Peroumal D, Abimannan T, Tagirasa R, et al. (August 2016). "Inherent low Erk and p38 activity reduce Fas Ligand expression and degranulation in T helper 17 cells leading to activation induced cell death resistance". Oncotarget. 7 (34): 54339–54359. doi:10.18632/oncotarget.10913. PMC 5342346. PMID 27486885.
- ^ Chiu YG, Ritchlin CT (January 2017). "Denosumab: targeting the RANKL pathway to treat rheumatoid arthritis". Expert Opinion on Biological Therapy. 17 (1): 119–128. doi:10.1080/14712598.2017.1263614. PMC 5794005. PMID 27871200.(subscription required)
- ^ Ideguchi H, Ohno S, Hattori H, et al. (2006). "Bone erosions in rheumatoid arthritis can be repaired through reduction in disease activity with conventional disease-modifying antirheumatic drugs". Arthritis Research & Therapy. 8 (3): R76. doi:10.1186/ar1943. PMC 1526642. PMID 16646983.
- ^ Takase-Minegishi K, Horita N, Kobayashi K, et al. (January 2018). "Diagnostic test accuracy of ultrasound for synovitis in rheumatoid arthritis: systematic review and meta-analysis". Rheumatology. 57 (1): 49–58. doi:10.1093/rheumatology/kex036. PMID 28340066.
- ^ Schueller-Weidekamm C (Apr 29, 2010). "Modern ultrasound methods yield stronger arthritis work-up". Diagnostic Imaging. 32. Archived from the original on April 9, 2019. Retrieved October 21, 2018.
- ^ Westwood OM, Nelson PN, Hay FC (April 2006). "Rheumatoid factors: what's new?". Rheumatology. 45 (4): 379–385. doi:10.1093/rheumatology/kei228. PMID 16418203.(subscription required)
- ^ Salman E, Çetiner S, Boral B, et al. (October 2019). "Importance of 14-3-3eta, anti-CarP, and anti-Sa in the diagnosis of seronegative rheumatoid arthritis". Turkish Journal of Medical Sciences. 49 (5): 1498–1502. doi:10.3906/sag-1812-137. PMC 7018368. PMID 31651120.
- ^ van Venrooij WJ, van Beers JJ, Pruijn GJ (June 2011). "Anti-CCP antibodies: the past, the present and the future". Nature Reviews. Rheumatology. 7 (7): 391–398. doi:10.1038/nrrheum.2011.76. PMID 21647203. S2CID 11858403.(subscription required)
- ^ Renger F, Bang H, Fredenhagen G, et al. "Anti-MCV Antibody Test for the Diagnosis of Rheumatoid Arthritis Using a POCT-Immunoassay". American College of Rheumatology, 2008 Annual Scientific Meeting, Poster Presentation. Archived from the original on 2010-05-27.
- ^ Luime JJ, Colin EM, Hazes JM, et al. (February 2010). "Does anti-mutated citrullinated vimentin have additional value as a serological marker in the diagnostic and prognostic investigation of patients with rheumatoid arthritis? A systematic review". Annals of the Rheumatic Diseases. 69 (2): 337–344. doi:10.1136/ard.2008.103283. PMID 19289382. S2CID 22283893.(subscription required)
- ^ Abdelhafiz D, Kilborn S, Bukhari M (June 2021). "The role of 14-3-3 η as a biomarker in rheumatoid arthritis". Rheumatology and Immunology Research. 2 (2): 87–90. doi:10.2478/rir-2021-0012. PMC 9524784. PMID 36465971. S2CID 238231522.
- ^ Barton JC, Barton JC (2015). "Autoimmune Conditions in 235 Hemochromatosis Probands with HFE C282Y Homozygosity and Their First-Degree Relatives". Journal of Immunology Research. 2015: 453046. doi:10.1155/2015/453046. PMC 4609477. PMID 26504855.
- ^ a b Aletaha D, Neogi T, Silman AJ, et al. (September 2010). "2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative" (PDF). Annals of the Rheumatic Diseases. 69 (9): 1580–1588. doi:10.1136/ard.2010.138461. hdl:2027.42/78045. PMID 20699241. S2CID 1191830.
- ^ Radu AF, Bungau SG (November 2021). "Management of Rheumatoid Arthritis: An Overview". Cells. 10 (11): 2857. doi:10.3390/cells10112857. ISSN 2073-4409. PMC 8616326. PMID 34831081.
- ^ Arnett FC, Edworthy SM, Bloch DA, et al. (March 1988). "The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis". Arthritis and Rheumatism. 31 (3): 315–34. doi:10.1002/art.1780310302. PMID 3358796.
- ^ Flynn JA, Choi MJ, Wooster DL (2013). Oxford American Handbook of Clinical Medicine. US: OUP. p. 400. ISBN 978-0-19-991494-4.
- ^ Seidman AJ, Limaiem F (2019). "Synovial Fluid Analysis". StatPearls. StatPearls Publishing. PMID 30725799. Retrieved 2019-12-19.
- ^ a b Berkow R, ed. (1992). The Merck Manual (16th ed.). Merck Publishing Group. pp. 1307–1308. ISBN 978-0-911910-16-2.(subscription required)
- ^ Roodenrijs NM, Welsing PM, van der Goes MC, et al. (December 2020). "Response to: 'Correspondence on EULAR definition of difficult-to-treat rheumatoid arthritis' by Novella-Navarro et al". Annals of the Rheumatic Diseases. 82 (3): annrheumdis–2020–219535. doi:10.1136/annrheumdis-2020-219535. hdl:1887/3594609. PMID 33277239. S2CID 227275679.
- ^ Raychaudhuri S (March 2010). "Recent advances in the genetics of rheumatoid arthritis". Current Opinion in Rheumatology. 22 (2): 109–118. doi:10.1097/bor.0b013e328336474d. PMC 3121048. PMID 20075733.
- ^ Conigliaro P, Triggianese P, De Martino E, et al. (July 2019). "Challenges in the treatment of Rheumatoid Arthritis". Autoimmunity Reviews. 18 (7): 706–713. doi:10.1016/j.autrev.2019.05.007. hdl:2108/225718. PMID 31059844. S2CID 146811143.
- ^ Conigliaro P, Ciccacci C, Politi C, et al. (2017-01-20). Ahuja SK (ed.). "Polymorphisms in STAT4, PTPN2, PSORS1C1 and TRAF3IP2 Genes Are Associated with the Response to TNF Inhibitors in Patients with Rheumatoid Arthritis". PLOS ONE. 12 (1): e0169956. Bibcode:2017PLoSO..1269956C. doi:10.1371/journal.pone.0169956. ISSN 1932-6203. PMC 5249113. PMID 28107378.
- ^ Klimenta B, Nefic H, Prodanovic N, et al. (December 2019). "Association of biomarkers of inflammation and HLA-DRB1 gene locus with risk of developing rheumatoid arthritis in females". Rheumatology International. 39 (12): 2147–2157. doi:10.1007/s00296-019-04429-y. PMID 31451934. S2CID 201644677.
- ^ Gregersen PK, Silver J, Winchester RJ (November 1987). "The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis". Arthritis and Rheumatism. 30 (11): 1205–1213. doi:10.1002/art.1780301102. PMID 2446635.
- ^ Kapitány A, Zilahi E, Szántó S, et al. (June 2005). "Association of rheumatoid arthritis with HLA-DR1 and HLA-DR4 in Hungary". Annals of the New York Academy of Sciences. 1051 (1): 263–270. Bibcode:2005NYASA1051..263K. doi:10.1196/annals.1361.067. PMID 16126967. S2CID 6515443.
- ^ Castro-Villegas C, Pérez-Sánchez C, Escudero A, et al. (March 2015). "Circulating miRNAs as potential biomarkers of therapy effectiveness in rheumatoid arthritis patients treated with anti-TNFα". Arthritis Research & Therapy. 17 (1): 49. doi:10.1186/s13075-015-0555-z (inactive 2024-09-12). PMC 4377058. PMID 25860297.
{{cite journal}}: CS1 maint: DOI inactive as of September 2024 (link) - ^ a b Prevoo ML, van 't Hof MA, Kuper HH, et al. (January 1995). "Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis". Arthritis and Rheumatism. 38 (1): 44–48. doi:10.1002/art.1780380107. hdl:2066/20651. PMID 7818570. S2CID 11192145.(subscription required)
- ^ Kelly, Janis (22 February 2005) DAS28 not always a reliable indicator of treatment effect in RA Archived 2011-02-25 at the Wayback Machine, Medscape Medical News.
- ^ Uribe L, Cerón C, Amariles P, et al. (July–September 2016). "Correlación entre la actividad clínica por DAS-28 y ecografía en pacientes con artritis reumatoide" [Correlation between clinical activity measured by DAS-28 and ultrasound in patients with rheumatoid arthritis]. Revista Colombiana de Reumatología (in Spanish). 23 (3): 159–169. doi:10.1016/j.rcreu.2016.05.002.
- ^ Yazici Y, Simsek I (January 2013). "Tools for monitoring remission in rheumatoid arthritis: any will do, let's just pick one and start measuring". Arthritis Research & Therapy. 15 (1): 104. doi:10.1186/ar4139. PMC 3672754. PMID 23374997.(subscription required)
- ^ Bruce B, Fries JF (June 2003). "The Stanford Health Assessment Questionnaire: dimensions and practical applications". Health and Quality of Life Outcomes. 1: 20. doi:10.1186/1477-7525-1-20. PMC 165587. PMID 12831398.(subscription required)
- ^ Saag KG, Teng GG, Patkar NM, et al. (June 2008). "American College of Rheumatology 2008 recommendations for the use of nonbiologic and biologic disease-modifying antirheumatic drugs in rheumatoid arthritis". Arthritis and Rheumatism. 59 (6): 762–784. doi:10.1002/art.23721. PMID 18512708.
- ^ Donahue KE, Schulman ER, Gartlehner G, et al. (October 2019). "Comparative Effectiveness of Combining MTX with Biologic Drug Therapy Versus Either MTX or Biologics Alone for Early Rheumatoid Arthritis in Adults: a Systematic Review and Network Meta-analysis". Journal of General Internal Medicine. 34 (10): 2232–2245. doi:10.1007/s11606-019-05230-0. PMC 6816735. PMID 31388915.
- ^ a b c Wasserman AM (December 2011). "Diagnosis and management of rheumatoid arthritis". American Family Physician. 84 (11): 1245–1252. PMID 22150658.
- ^ Donahue KE, Gartlehner G, Schulman ER, et al. (2018-07-16). "Drug Therapy for Early Rheumatoid Arthritis: A Systematic Review Update". Effective Health Care Program. doi:10.23970/ahrqepccer211. S2CID 81414779.[permanent dead link]
- ^ Richards BL, Whittle SL, Buchbinder R (January 2012). Richards BL (ed.). "Muscle relaxants for pain management in rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 1: CD008922. doi:10.1002/14651858.CD008922.pub2. PMID 22258993. S2CID 73769165.
- ^ Hurkmans E, van der Giesen FJ, Vliet Vlieland TP, et al. (October 2009). Hurkmans E (ed.). "Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2009 (4): CD006853. doi:10.1002/14651858.CD006853.pub2. PMC 6769170. PMID 19821388.
- ^ Cramp F, Hewlett S, Almeida C, et al. (August 2013). "Non-pharmacological interventions for fatigue in rheumatoid arthritis". The Cochrane Database of Systematic Reviews (8): CD008322. doi:10.1002/14651858.CD008322.pub2. PMID 23975674.
- ^ Williams MA, Srikesavan C, Heine PJ, et al. (July 2018). "Exercise for rheumatoid arthritis of the hand". The Cochrane Database of Systematic Reviews. 2018 (7): CD003832. doi:10.1002/14651858.cd003832.pub3. PMC 6513509. PMID 30063798.
- ^ Jabeen A (16 August 2023). "The Benefits of Exercise in Rheumatoid Arthritis: A Comprehensive Guide". rheumatologydelaware. Attiya Jabeen. Archived from the original on 1 November 2023. Retrieved August 16, 2023.
- ^ Rausch Osthoff AK, Juhl CB, Knittle K, et al. (December 2018). "Effects of exercise and physical activity promotion: meta-analysis informing the 2018 EULAR recommendations for physical activity in people with rheumatoid arthritis, spondyloarthritis and hip/knee osteoarthritis". RMD Open. 4 (2): e000713. doi:10.1136/rmdopen-2018-000713. PMC 6307596. PMID 30622734.
- ^ Hagen KB, Byfuglien MG, Falzon L, et al. (January 2009). Hagen KB (ed.). "Dietary interventions for rheumatoid arthritis". The Cochrane Database of Systematic Reviews (1): CD006400. doi:10.1002/14651858.CD006400.pub2. PMID 19160281.
- ^ Steultjens EM, Dekker J, Bouter LM, et al. (2004). "Occupational therapy for rheumatoid arthritis" (PDF). The Cochrane Database of Systematic Reviews. 2004 (1): CD003114. doi:10.1002/14651858.CD003114.pub2. hdl:2066/58846. PMC 7017227. PMID 14974005.
- ^ Robinson V, Brosseau L, Casimiro L, et al. (2002-04-22). "Thermotherapy for treating rheumatoid arthritis". The Cochrane Database of Systematic Reviews (2): CD002826. doi:10.1002/14651858.cd002826. PMC 6991938. PMID 12076454.
- ^ Riemsma RP, Kirwan JR, Taal E, et al. (2003-04-22). "Patient education for adults with rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2009 (2): CD003688. doi:10.1002/14651858.cd003688. PMID 12804484.
- ^ a b Egan M, Brosseau L, Farmer M, et al. (2001-10-23). "Splints/orthoses in the treatment of rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2001 (1): CD004018. doi:10.1002/14651858.cd004018. PMC 8762649. PMID 12535502.
- ^ Isaacs D (2010-07-07). "Tocilizumab for rheumatoid arthritis". In Singh JA (ed.). Cochrane Database of Systematic Reviews. Advances in Experimental Medicine and Biology. Vol. 764. John Wiley & Sons. pp. 151–158. doi:10.1002/14651858.cd008331.pub2. PMID 23654064.
- ^ Osiri M, Shea B, Robinson V, et al. (2003). "Leflunomide for treating rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2002 (1): CD002047. doi:10.1002/14651858.CD002047. PMC 8437750. PMID 12535423.
- ^ Suarez-Almazor ME, Belseck E, Shea B, et al. (1998-04-27). "Sulfasalazine for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 1998 (2): CD000958. doi:10.1002/14651858.cd000958. PMC 7047550. PMID 10796400.
- ^ Suarez-Almazor ME, Belseck E, Shea B, et al. (2000). "Antimalarials for treating rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2010 (4): CD000959. doi:10.1002/14651858.CD000959. PMC 8407035. PMID 11034691.
- ^ Katchamart W, Trudeau J, Phumethum V, et al. (April 2010). "Methotrexate monotherapy versus methotrexate combination therapy with non-biologic disease modifying anti-rheumatic drugs for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2015 (4): CD008495. doi:10.1002/14651858.cd008495. PMC 8946299. PMID 20393970.
- ^ a b c DiPiro JT, Talbert RL, Yee GC, et al. (2008). Pharmacotherapy: a Pathophysiologic Approach (7th ed.). New York: McGraw-Hill. ISBN 978-0-07-147899-1.
- ^ Singh JA, Hossain A, Mudano AS, et al. (May 2017). "Biologics or tofacitinib for people with rheumatoid arthritis naive to methotrexate: a systematic review and network meta-analysis". The Cochrane Database of Systematic Reviews. 2017 (5): CD012657. doi:10.1002/14651858.cd012657. PMC 6481641. PMID 28481462.
- ^ Hazlewood GS, Barnabe C, Tomlinson G, et al. (August 2016). "Methotrexate monotherapy and methotrexate combination therapy with traditional and biologic disease modifying anti-rheumatic drugs for rheumatoid arthritis: A network meta-analysis". The Cochrane Database of Systematic Reviews. 2016 (8): CD010227. doi:10.1002/14651858.cd010227.pub2. PMC 7087436. PMID 27571502.
- ^ Shea B, Swinden MV, Tanjong Ghogomu E, et al. (May 2013). "Folic acid and folinic acid for reducing side effects in patients receiving methotrexate for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 5 (5): CD000951. doi:10.1002/14651858.CD000951.pub2. PMC 7046011. PMID 23728635.
- ^ a b Lopez-Olivo MA, Amezaga Urruela M, McGahan L, et al. (January 2015). "Rituximab for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 1 (1): CD007356. doi:10.1002/14651858.CD007356.pub2. PMC 11115378. PMID 25603545.
- ^ Singh JA, Cameron C, Noorbaloochi S, et al. (July 2015). "Risk of serious infection in biological treatment of patients with rheumatoid arthritis: a systematic review and meta-analysis". Lancet. 386 (9990): 258–265. doi:10.1016/S0140-6736(14)61704-9. PMC 4580232. PMID 25975452.
- ^ Singh JA, Hossain A, Tanjong Ghogomu E, et al. (November 2016). "Biologic or tofacitinib monotherapy for rheumatoid arthritis in people with traditional disease-modifying anti-rheumatic drug (DMARD) failure: a Cochrane Systematic Review and network meta-analysis (NMA)". The Cochrane Database of Systematic Reviews. 2016 (11): CD012437. doi:10.1002/14651858.cd012437. PMC 6469573. PMID 27855242.
- ^ Singh JA, Hossain A, Tanjong Ghogomu E, et al. (March 2017). "Biologics or tofacitinib for people with rheumatoid arthritis unsuccessfully treated with biologics: a systematic review and network meta-analysis". The Cochrane Database of Systematic Reviews. 2017 (3): CD012591. doi:10.1002/14651858.cd012591. PMC 6472522. PMID 28282491.
- ^ Maxwell L, Singh JA (October 2009). "Abatacept for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2009 (4): CD007277. doi:10.1002/14651858.CD007277.pub2. PMC 6464777. PMID 19821401.
- ^ a b Verhoef LM, van den Bemt BJ, van der Maas A, et al. (May 2019). "Down-titration and discontinuation strategies of tumour necrosis factor-blocking agents for rheumatoid arthritis in patients with low disease activity". The Cochrane Database of Systematic Reviews. 5 (6): CD010455. doi:10.1002/14651858.CD010455.pub3. PMC 6534285. PMID 31125448.
- ^ Donahue KE, Gartlehner G, Schulman ER, et al. (2018-07-16). Drug Therapy for Early Rheumatoid Arthritis: A Systematic Review Update (Report). Agency for Healthcare Research and Quality (AHRQ). doi:10.23970/ahrqepccer211.
- ^ Singh JA, Noorbaloochi S, Singh G (January 2010). "Golimumab for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2010 (1): CD008341. doi:10.1002/14651858.CD008341. PMC 10732339. PMID 20091667.
- ^ Aaltonen KJ, Virkki LM, Malmivaara A, et al. (2012). Hernandez AV (ed.). "Systematic review and meta-analysis of the efficacy and safety of existing TNF blocking agents in treatment of rheumatoid arthritis". PLOS ONE. 7 (1): e30275. Bibcode:2012PLoSO...730275A. doi:10.1371/journal.pone.0030275. PMC 3260264. PMID 22272322.
- ^ Lethaby A, Lopez-Olivo MA, Maxwell L, et al. (May 2013). "Etanercept for the treatment of rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2014 (5): CD004525. doi:10.1002/14651858.cd004525.pub2. PMC 10771320. PMID 23728649.
- ^ Maxwell L, Singh JA (October 2009). Maxwell L (ed.). "Abatacept for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2009 (4): CD007277. doi:10.1002/14651858.CD007277.pub2. PMC 6464777. PMID 19821401.
- ^ Navarro-Sarabia F, Ariza-Ariza R, Hernandez-Cruz B, et al. (July 2005). "Adalimumab for treating rheumatoid arthritis". The Cochrane Database of Systematic Reviews (3): CD005113. doi:10.1002/14651858.CD005113.pub2. PMID 16034967.
- ^ Singh JA, Christensen R, Wells GA, et al. (October 2009). Singh JA (ed.). "Biologics for rheumatoid arthritis: an overview of Cochrane reviews". The Cochrane Database of Systematic Reviews (Submitted manuscript). 128 (4): CD007848. doi:10.1002/14651858.CD007848.pub2. PMC 10636593. PMID 19821440.
- ^ a b Almeida C, Choy EH, Hewlett S, et al. (June 2016). "Biologic interventions for fatigue in rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2016 (6): CD008334. doi:10.1002/14651858.cd008334.pub2. PMC 7175833. PMID 27271314.
- ^ Wells G, Haguenauer D, Shea B, et al. (2000). "Cyclosporine for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 1998 (2): CD001083. doi:10.1002/14651858.CD001083. PMC 8406939. PMID 10796412.
- ^ Criswell LA, Saag KG, Sems KM, et al. (1998-07-27). "Moderate-term, low-dose corticosteroids for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2010 (2): CD001158. doi:10.1002/14651858.cd001158. PMC 8406983. PMID 10796420.
- ^ Kirwan JR, Bijlsma JW, Boers M, et al. (January 2007). "Effects of glucocorticoids on radiological progression in rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2010 (1): CD006356. doi:10.1002/14651858.cd006356. PMC 6465045. PMID 17253590.
- ^ Wallen M, Gillies D (January 2006). "Intra-articular steroids and splints/rest for children with juvenile idiopathic arthritis and adults with rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2008 (1): CD002824. doi:10.1002/14651858.cd002824.pub2. PMC 8453330. PMID 16437446.
- ^ a b Ramiro S, Radner H, van der Heijde D, et al. (October 2011). "Combination therapy for pain management in inflammatory arthritis (rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, other spondyloarthritis)". The Cochrane Database of Systematic Reviews (10): CD008886. doi:10.1002/14651858.cd008886.pub2. PMID 21975788.
- ^ Tarp S, Bartels EM, Bliddal H, et al. (November 2012). "Effect of nonsteroidal antiinflammatory drugs on the C-reactive protein level in rheumatoid arthritis: a meta-analysis of randomized controlled trials". Arthritis and Rheumatism. 64 (11): 3511–3521. doi:10.1002/art.34644. PMID 22833186.
- ^ Radner H, Ramiro S, Buchbinder R, et al. (January 2012). Radner H (ed.). "Pain management for inflammatory arthritis (rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and other spondylarthritis) and gastrointestinal or liver comorbidity". The Cochrane Database of Systematic Reviews. 1 (2): CD008951. doi:10.1002/14651858.CD008951.pub2. PMC 8950811. PMID 22258995.
- ^ McCormack PL (December 2011). "Celecoxib: a review of its use for symptomatic relief in the treatment of osteoarthritis, rheumatoid arthritis and ankylosing spondylitis". Drugs. 71 (18): 2457–2489. doi:10.2165/11208240-000000000-00000. PMID 22141388. S2CID 71357689.
- ^ Marks JL, Colebatch AN, Buchbinder R, et al. (October 2011). Marks JL (ed.). "Pain management for rheumatoid arthritis and cardiovascular or renal comorbidity". The Cochrane Database of Systematic Reviews (10): CD008952. doi:10.1002/14651858.CD008952.pub2. PMID 21975789.
- ^ Garner SE, Fidan DD, Frankish RR, et al. (January 2005). "Rofecoxib for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2010 (1): CD003685. doi:10.1002/14651858.cd003685.pub2. PMC 8725608. PMID 15674912.
- ^ Colebatch AN, Marks JL, Edwards CJ (November 2011). "Safety of non-steroidal anti-inflammatory drugs, including aspirin and paracetamol (acetaminophen) in people receiving methotrexate for inflammatory arthritis (rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, other spondyloarthritis)". The Cochrane Database of Systematic Reviews (11): CD008872. doi:10.1002/14651858.CD008872.pub2. PMID 22071858.
- ^ Chen YF, Jobanputra P, Barton P, et al. (April 2008). "Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation". Health Technology Assessment. 12 (11): 1–278, iii. doi:10.3310/hta12110. PMID 18405470.
- ^ Fidahic M, Jelicic Kadic A, Radic M, et al. (June 2017). "Celecoxib for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2017 (6): CD012095. doi:10.1002/14651858.CD012095.pub2. PMC 6481589. PMID 28597983.
- ^ a b Wienecke T, Gøtzsche PC (2004-01-26). "Paracetamol versus nonsteroidal anti-inflammatory drugs for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2010 (1): CD003789. doi:10.1002/14651858.cd003789.pub2. PMC 8730319. PMID 14974037.
- ^ a b Richards BL, Whittle SL, Buchbinder R (January 2012). "Neuromodulators for pain management in rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 1 (1): CD008921. doi:10.1002/14651858.CD008921.pub2. PMC 6956614. PMID 22258992.
- ^ Whittle SL, Richards BL, Husni E, et al. (November 2011). "Opioid therapy for treating rheumatoid arthritis pain". The Cochrane Database of Systematic Reviews (11): CD003113. doi:10.1002/14651858.cd003113.pub3. PMID 22071805.
- ^ Christie A, Dagfinrud H, Engen Matre K, et al. (January 2010). "Surgical interventions for the rheumatoid shoulder". The Cochrane Database of Systematic Reviews (1): CD006188. doi:10.1002/14651858.cd006188.pub2. PMID 20091587.
- ^ a b Kavuncu V, Evcik D (May 2004). "Physiotherapy in rheumatoid arthritis". MedGenMed. 6 (2): 3. PMC 1395797. PMID 15266230.
- ^ a b Hammond A, Prior Y (September 2016). "The effectiveness of home hand exercise programmes in rheumatoid arthritis: a systematic review". British Medical Bulletin. 119 (1): 49–62. doi:10.1093/bmb/ldw024. PMID 27365455.
- ^ a b Peres D, Sagawa Y, Dugué B, et al. (October 2017). "The practice of physical activity and cryotherapy in rheumatoid arthritis: systematic review". European Journal of Physical and Rehabilitation Medicine. 53 (5): 775–787. doi:10.23736/s1973-9087.16.04534-2. PMID 27996221.
- ^ Hammond A, Prior Y (1 March 2021). "Compression gloves for patients with hand arthritis (C-GLOVES): A feasibility study". Hand Therapy. 26 (1): 26–37. doi:10.1177/1758998320986829. ISSN 1758-9983. PMC 10584057. PMID 37905193. S2CID 232050521.
- ^ Hammond A, Jones V, Prior Y (March 2016). "The effects of compression gloves on hand symptoms and hand function in rheumatoid arthritis and hand osteoarthritis: a systematic review" (PDF). Clinical Rehabilitation. 30 (3): 213–224. doi:10.1177/0269215515578296. PMID 25802424. S2CID 40742720.
- ^ "Rheumatoid Arthritis and Complementary Health Approaches". National Center for Complementary and Integrative Health. January 2006. Archived from the original on July 5, 2015. Retrieved July 1, 2015.
- ^ Macfarlane GJ, El-Metwally A, De Silva V, et al. (Arthritis Research UK Working Group on Complementary Alternative Medicines) (September 2011). "Evidence for the efficacy of complementary and alternative medicines in the management of rheumatoid arthritis: a systematic review". Rheumatology. 50 (9): 1672–1683. doi:10.1093/rheumatology/ker119. PMID 21652584.
- ^ a b Efthimiou P, Kukar M (March 2010). "Complementary and alternative medicine use in rheumatoid arthritis: proposed mechanism of action and efficacy of commonly used modalities". Rheumatology International. 30 (5): 571–586. doi:10.1007/s00296-009-1206-y. PMID 19876631. S2CID 21179821.
- ^ Brosseau L, Robinson V, Wells G, et al. (October 2005). "Low level laser therapy (Classes I, II and III) for treating rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 4 (4): CD002049. doi:10.1002/14651858.CD002049.pub2. PMC 8406947. PMID 16235295.
- ^ Mudano AS, Tugwell P, Wells GA, et al. (September 2019). "Tai Chi for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 9 (9): CD004849. doi:10.1002/14651858.CD004849.pub2. PMC 6759565. PMID 31553478.
- ^ Lee MS, Pittler MH, Ernst E (November 2007). "Tai chi for rheumatoid arthritis: systematic review". Rheumatology. 46 (11): 1648–1651. doi:10.1093/rheumatology/kem151. PMID 17634188.
- ^ Lee MS, Shin BC, Ernst E (December 2008). "Acupuncture for rheumatoid arthritis: a systematic review". Rheumatology. 47 (12): 1747–1753. doi:10.1093/rheumatology/ken330. PMID 18710899.
- ^ Macfarlane GJ, Paudyal P, Doherty M, et al. (Arthritis Research UK Working Group on Complementary Alternative Therapies for the Management of the Rheumatic Diseases) (September 2012). "A systematic review of evidence for the effectiveness of practitioner-based complementary and alternative therapies in the management of rheumatic diseases: rheumatoid arthritis". Rheumatology. 51 (9): 1707–1713. doi:10.1093/rheumatology/kes133. PMID 22661556.
- ^ Brosseau LU, Pelland LU, Casimiro LY, et al. (2002). "Electrical stimulation for the treatment of rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2010 (2): CD003687. doi:10.1002/14651858.CD003687. PMC 8725644. PMID 12076504.
- ^ Suarez-Almazor ME, Spooner C, Belseck E (2000-10-23). "Penicillamine for treating rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2011 (4): CD001460. doi:10.1002/14651858.cd001460. PMC 8407185. PMID 11034719.
- ^ a b Casimiro L, Brosseau L, Robinson V, et al. (2002-07-22). "Therapeutic ultrasound for the treatment of rheumatoid arthritis". The Cochrane Database of Systematic Reviews (3): CD003787. doi:10.1002/14651858.cd003787. PMID 12137714.
- ^ a b Johnson MI, Walsh DM (June 2010). "Pain: continued uncertainty of TENS' effectiveness for pain relief". Nature Reviews. Rheumatology. 6 (6): 314–316. doi:10.1002/14651858.cd004377. PMC 8826159. PMID 20520646.
- ^ a b Tuntland H, Kjeken I, Nordheim LV, et al. (October 2009). "Assistive technology for rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2009 (4): CD006729. doi:10.1002/14651858.cd006729.pub2. PMC 7389411. PMID 19821383.
- ^ Silva KN, Mizusaki Imoto A, Almeida GJ, et al. (May 2010). "Balance training (proprioceptive training) for patients with rheumatoid arthritis". The Cochrane Database of Systematic Reviews (5): CD007648. doi:10.1002/14651858.cd007648.pub2. PMID 20464755.
- ^ Martin RH (May 1998). "The role of nutrition and diet in rheumatoid arthritis". The Proceedings of the Nutrition Society. 57 (2): 231–234. doi:10.1079/pns19980036 (inactive 2024-08-01). PMID 9656325. S2CID 2000161.
{{cite journal}}: CS1 maint: DOI inactive as of August 2024 (link) - ^ Tedeschi SK, Costenbader KH (May 2016). "Is There a Role for Diet in the Therapy of Rheumatoid Arthritis?". Current Rheumatology Reports. 18 (5): 23. doi:10.1007/s11926-016-0575-y. PMID 27032786. S2CID 39883142.
- ^ Soeken KL, Miller SA, Ernst E (May 2003). "Herbal medicines for the treatment of rheumatoid arthritis: a systematic review". Rheumatology. 42 (5). National Institute for Health and Care Research: 652–659. doi:10.1093/rheumatology/keg183. PMID 12709541. Archived from the original on January 16, 2014. Retrieved March 23, 2013.
- ^ a b Senftleber NK, Nielsen SM, Andersen JR, et al. (January 2017). "Marine Oil Supplements for Arthritis Pain: A Systematic Review and Meta-Analysis of Randomized Trials". Nutrients. 9 (1): 42. doi:10.3390/nu9010042. PMC 5295086. PMID 28067815.
- ^ a b Jiang J, Li K, Wang F, et al. (2016). "Effect of Marine-Derived n-3 Polyunsaturated Fatty Acids on Major Eicosanoids: A Systematic Review and Meta-Analysis from 18 Randomized Controlled Trials". PLOS ONE. 11 (1): e0147351. Bibcode:2016PLoSO..1147351J. doi:10.1371/journal.pone.0147351. PMC 4726565. PMID 26808318.
- ^ a b Di Giuseppe D, Crippa A, Orsini N, et al. (September 2014). "Fish consumption and risk of rheumatoid arthritis: a dose-response meta-analysis". Arthritis Research & Therapy. 16 (5): 446. doi:10.1186/s13075-014-0446-8. PMC 4201724. PMID 25267142.
- ^ a b Lee YH, Bae SC, Song GG (July 2012). "Omega-3 polyunsaturated fatty acids and the treatment of rheumatoid arthritis: a meta-analysis". Archives of Medical Research. 43 (5): 356–362. doi:10.1016/j.arcmed.2012.06.011. PMID 22835600.
- ^ a b "Herbal Remedies, Supplements and Acupuncture for Arthritis". American College of Rheumatology. Archived from the original on May 5, 2013. Retrieved May 3, 2013.
- ^ Gotzsche PC, Johansen HK (2005-01-24). "Short-term low-dose corticosteroids vs placebo and nonsteroidal antiinflammatory drugs in rheumatoid arthritis". The Cochrane Database of Systematic Reviews. 2005 (3): CD000189. doi:10.1002/14651858.cd000189.pub2. PMC 7043293. PMID 15266426.
- ^ Perry LM, Winthrop KL, Curtis JR (August 2014). "Vaccinations for rheumatoid arthritis". Current Rheumatology Reports. 16 (8): 431. doi:10.1007/s11926-014-0431-x. PMC 4080407. PMID 24925587.
- ^ Grohskopf LA, Olsen SJ, Sokolow LZ, et al. (August 2014). "Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP) -- United States, 2014-15 influenza season". MMWR. Morbidity and Mortality Weekly Report. 63 (32): 691–697. PMC 4584910. PMID 25121712.
- ^ Black CL, Yue X, Ball SW, et al. (September 2014). "Influenza vaccination coverage among health care personnel--United States, 2013-14 influenza season". MMWR. Morbidity and Mortality Weekly Report. 63 (37): 805–811. PMC 5779456. PMID 25233281.
- ^ Hales CM, Harpaz R, Ortega-Sanchez I, et al. (August 2014). "Update on recommendations for use of herpes zoster vaccine". MMWR. Morbidity and Mortality Weekly Report. 63 (33): 729–731. PMC 5779434. PMID 25144544.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on November 11, 2009. Retrieved November 11, 2009.
- ^ Carlson KJ, Eisenstat SA, Ziporyn TD (2004). The New Harvard Guide to Women's Health. Cambridge, MA: Harvard University Press – via Credo Reference.
- ^ Ali N (2013). Arthritis and You. Lanham, MD: Rowman & Littlefield Publishers, Inc. pp. 138. ISBN 978-1-4422-1901-4.
- ^ Carrier N, Brum-Fernanades AJ, Liang P, et al. (April 2020). "Impending radiographic erosive progression over the following year in a cohort of consecutive patients with inflammatory polyarthritis: prediction by serum biomarkers". RMD Open. 6 (1): e001191. doi:10.1136/rmdopen-2020-001191. PMC 7299510. PMID 32371434.
- ^ Carrier N, Marotta A, Brum-Fernanades AJ, et al. (Feb 2016). "Serum levels of 14-3-3η protein supplement C-reactive protein and rheumatoid arthritis-associated antibodies to predict clinical and radiographic outcomes in a prospective cohort of patients with recent-onset inflammatory polyarthritis". Arthritis Research & Therapy. 18 (37): 37. doi:10.1186/s13075-016-0935-z (inactive 2024-09-12). PMC 4736641. PMID 26832367.
{{cite journal}}: CS1 maint: DOI inactive as of September 2024 (link) - ^ Kitas, George (4 April 2006) Why is life span shortened by Rheumatoid Arthritis? National Rheumatoid Arthritis Society
- ^ Rheumatoid Arthritis Patients Have Double the Risk of Heart Failure. mayoclinic.org (3 February 2005).
- ^ "Cardiac disease in rheumatoid arthritis". Johns Hopkins University. 2002. Archived from the original on October 9, 2006.
- ^ Atzeni F, Turiel M, Caporali R, et al. (October 2010). "The effect of pharmacological therapy on the cardiovascular system of patients with systemic rheumatic diseases". Autoimmunity Reviews. 9 (12): 835–839. doi:10.1016/j.autrev.2010.07.018. PMID 20678592.
- ^ Damjanov N, Nurmohamed MT, Szekanecz Z (March 2014). "Biologics, cardiovascular effects and cancer". BMC Medicine. 12 (1): 48. doi:10.1186/1741-7015-12-48. PMC 3984692. PMID 24642038.
- ^ Lozano R, Naghavi M, Foreman K, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–2128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMC 10790329. PMID 23245604. S2CID 1541253.
- ^ Alamanos Y, Voulgari PV, Drosos AA (December 2006). "Incidence and prevalence of rheumatoid arthritis, based on the 1987 American College of Rheumatology criteria: a systematic review". Seminars in Arthritis and Rheumatism. 36 (3): 182–188. doi:10.1016/j.semarthrit.2006.08.006. PMID 17045630.
- ^ "Rheumatoid Arthritis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 2017-04-20. Retrieved 2024-09-26.
- ^ Shammas RM, Ranganath VK, Paulus HE (2010). "Remission in Rheumatoid Arthritis". Current Rheumatology Reports. 12 (5): 355–362. doi:10.1007/s11926-010-0121-2. PMC 2927687. PMID 20697983.
- ^ Watson S (2024-08-13). "Progression of Rheumatoid Arthritis". WebMD. Retrieved 2024-09-26.
- ^ "Rheumatoid Arthritis (RA): Causes, Symptoms & Treatment FAQs". Cleveland Clinic. 2023-08-31. Retrieved 2024-09-26.
- ^ Cheng Z, Meade J, Mankia K, et al. (February 2017). "Periodontal disease and periodontal bacteria as triggers for rheumatoid arthritis" (PDF). Best Practice & Research. Clinical Rheumatology. 31 (1): 19–30. doi:10.1016/j.berh.2017.08.001. PMID 29221594.
- ^ Garrod AB (1859). The Nature and Treatment of Gout and Rheumatic Gout. London: Walton and Maberly.
- ^ Appelboom T, de Boelpaepe C, Ehrlich GE, et al. (February 1981). "Rubens and the question of antiquity of rheumatoid arthritis". JAMA. 245 (5): 483–486. doi:10.1001/jama.245.5.483. PMID 7005475.
- ^ Kelly J (14 June 2005). "Did RA travel from New World to Old? The Rubens connection". Medscape. Archived from the original on 15 December 2013. Retrieved March 3, 2011.
- ^ Dequeker J, Rico H (July 1992). "Rheumatoid arthritis-like deformities in an early 16th-century painting of the Flemish-Dutch school". JAMA. 268 (2): 249–251. doi:10.1001/jama.268.2.249. PMID 1608144.
- ^ Hart FD (March 1976). "History of the treatment of rheumatoid arthritis". British Medical Journal. 1 (6012): 763–765. doi:10.1136/bmj.1.6012.763. PMC 1639217. PMID 177148.
- ^ Tang Q, Fu H, Qin B, et al. (2017-02-01). "A Possible Link Between Rheumatoid Arthritis and Periodontitis: A Systematic Review and Meta-analysis". The International Journal of Periodontics & Restorative Dentistry. 37 (1): 79–86. doi:10.11607/prd.2656. PMID 27977821.
- ^ Gatenby P, Lucas R, Swaminathan A (March 2013). "Vitamin D deficiency and risk for rheumatic diseases: an update". Current Opinion in Rheumatology. 25 (2): 184–191. doi:10.1097/BOR.0b013e32835cfc16. PMID 23370372. S2CID 10851180.
- ^ Wen H, Baker JF (March 2011). "Vitamin D, immunoregulation, and rheumatoid arthritis". Journal of Clinical Rheumatology. 17 (2): 102–107. doi:10.1097/RHU.0b013e31820edd18. PMID 21364350. S2CID 25831521.
- ^ Guillot X, Semerano L, Saidenberg-Kermanac'h N, et al. (December 2010). "Vitamin D and inflammation". Joint, Bone, Spine. 77 (6): 552–557. doi:10.1016/j.jbspin.2010.09.018. PMID 21067953.
- ^ Lee YH, Bae SC (2016). "Vitamin D level in rheumatoid arthritis and its correlation with the disease activity: a meta-analysis". Clinical and Experimental Rheumatology. 34 (5): 827–833. PMID 27049238. Archived from the original on 2017-04-05.
- ^ Matei DE, Menon M, Alber DG, et al. (July 2021). "Intestinal barrier dysfunction plays an integral role in arthritis pathology and can be targeted to ameliorate disease". Med. 2 (7): 864–883.e9. doi:10.1016/j.medj.2021.04.013. PMC 8280953. PMID 34296202.
External links
[edit]- "Rheumatoid Arthritis". MedlinePlus. U.S. National Library of Medicine.



